The Prostate Cancer Diagnosis Battle on All Gender Fronts
Both cis and transgender individuals face invasive screening and diagnostic delays when it comes to prostate cancer – isn’t there a better way?
Jessica Allerton | | 4 min read | Discussion

In recent months, two of the men nearest and dearest to me were diagnosed with prostate cancer and, though they were fortunate enough to be diagnosed in the early stages, they will never be free from the clutches of the disease. After being told “You’re more likely to die with it than from it” and learning that they’ll have frequent hospital appointments for the rest of their lives, I’m left wondering: why are we still so far behind in prostate cancer research?
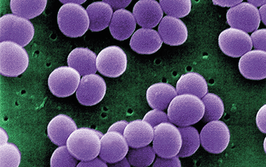
In fact, one in eight men will have prostate cancer in their lifetimes (1), but, despite this high statistic, there is still no singular test for diagnosis – and there is a lot we still don’t know about this disease. Why, with such a large proportion of the population battling with prostate cancer, are the efforts of researchers and clinicians still falling short?
One barrier involves the slow development of the disease; it could take years before the patient notices any signs or changes to their body (2). Moreover, we’ve all heard the stereotype: “men won’t book a doctor’s appointment unless absolutely necessary.” But is it just a stereotype? Statistics show that one in five untested males aren’t willing to go for a routine prostate checkup (3). Of course, prostate screenings are quite invasive and many people have to mentally overcome fears of emasculation to book and attend appointments (4). However, despite the uncomfortable experience, we must encourage our menfolk to consider that a couple minutes of unease is preferable to remaining unaware of a hidden cancer.
But what about transgender women? Disparities in transgender and gender-expansive patient care – from cervical cancer screenings to prostate exams – is a prominent issue in healthcare (5). Much of this disparity could stem from a lack of communication between healthcare professionals and patients. For example, transgender women keep their prostates following gender-affirming surgery, which keeps them at risk for prostate cancer. By counseling transgender individuals to be up to date on important screenings, such as pap smears and prostate exams, regardless of gender, we could have a positive impact. Updating electronic medical records when relevant to allow for the capture of affirmed gender identity data would also help.
One recent study showed that transgender women receiving estrogen scored 50 times lower than average on prostate-specific antigen (PSA) tests (6), which could give false reassurance and a delay in diagnosis and treatment. This research suggests that the presence of gender-affirming hormones, though essential to the physical and mental health of transgender women, could be seriously impeding prostate cancer diagnosis. It seems clear that we need more research into how estrogen and related treatments modulate prostate cancer risk.
“As more and more transwomen have appropriate access to gender-affirming care, it’s critical not to lose sight of long-term cancer risks in retained organs,” says Matthew R. Cooperberg, UCSF urology professor and co-leader of the prostate cancer program at the UCSF Helen Diller Family Comprehensive Cancer Center (7).
This statement insinuates that it’s not only patient awareness but also clinician knowledge that is crucial in the battle against prostate cancer for both cis and transgender individuals. The World Professional Association for Transgender Health (WPATH) has also commented on the crucial elements of clinical health regardless of gender, stating, “Being transsexual, transgender, or gender non-conforming is a matter of diversity, not pathology (8).”
Going back to diagnostics, we need to develop alternate screening tests for prostate cancer that are significantly less invasive than current procedures – for everyone.
Back in February 2020, urine-based assays showed promise for the diagnosis and classification of prostate cancer (9). The study aimed to develop algorithms to identify prostate cancer across risk groups through three assays, but the resulting data brought up more questions rather than definitive answers.
Since then, we’ve seen further promising studies, including lipidomic profiling with quantitative mass spectrometry to reveal targetable alterations in prostate cancer membrane lipid composition (10) and a combined imaging and biopsy diagnostic approach (11). And in January 2024, researchers developed a cell-free DNA targeted methylation plasma panel to detect castration-resistant neuroendocrine prostate cancer (CRPC-NE).
There’s still a long way to go before standard testing evolves from the current prostate screening exam, but I’m sure we can all hope for a more inclusive and less invasive diagnostic future for prostate cancer.
- Prostate Cancer UK (2024). Available at: https://prostatecanceruk.org/
- NHS, “Prostate Cancer” (2024). Available at: https://www.nhs.uk/conditions/prostate-cancer/
- YouGov (2021). Available at: https://yougov.co.uk/health/articles/39607-prostate-cancer-two-thirds-british-males-dont-know
- LJ James et al., PLoS One, 12, 11 (2017). PMID: 29182649.
- Critical Values (2023). Available at: https://www.criticalvalues.org/news/item/2023/06/06/pathology-and-transgender-care-what-has-changed-in-the-past-decade-and-where-are-we-heading
- F Nik-Ahd et al., JAMA (2024). PMID: 38922607.
- News-Medical Life Sciences (2024). Available at: https://www.news-medical.net/news/20240628/Study-alerts-transwomen-to-interpret-standard-prostate-cancer-screening-guidelines-with-caution.aspx#:~:text=%22As%20more%20and%20more%20transwomen,the%20UCSF%20Helen%20Diller%20Family
- J Morgan, Lancet Psychiatry, 2, 2 (2015). PMID: 26359743
- ASCO Daily News (2020). Available at: https://dailynews.ascopubs.org/do/urine-based-rna-assays-show-promise-diagnosis-classification-prostate-cancer
- LM Butlet et al., Cancer Res, 81, 19 (2021). PMID: 34362796.
- D Qiu et al., ASCO Publications, 40, 6 (2022). PMID: 34860277.
- GM Franceschini et al., Cancer Discov, 14, 3 (2024). PMID: 38197680.
Deputy Editor, The Pathologist