Into the Multi-ome
What simultaneously sequencing four ‘omes could mean for the future of personalized healthcare
Mark van Oene | | 4 min read | Discussion

Credit: Mark van Oene
Biology is a complex and multi-layered system, with many interdependent pathways taking place in concert. The first (and therefore arguably the most influential) biological layer is the genome. Fuelled by advances in technology, our understanding of the genome has grown significantly in recent years. This has led to breakthroughs including the completion of the entire human genome by the Telomere-to-Telomere Consortium (1), but a world of insight beyond the genome still remains unassessed. For example, only 50 percent of rare disease patients receive a diagnosis even after short-read whole genome sequencing (2). This leads us to believe that the cause of these conditions is hidden in another layer of our biology.
Moving forward with our new ability to explore the molecular universe, researchers can use sequencing technology to explore the four ‘omes that we know are highly relevant to biological function: the genome, transcriptome, methylome, and chromatin epigenome. Together, this “multi-ome” is providing researchers with new insights into the mechanisms of life and disease.
There are many instances where analyzing the genome provides adequate insight for researchers. But with complex cases, a deeper level of biological exploration is necessary. In the building blocks of life, the genome acts as a foundational blueprint to instruct biological processes in the body – from our eye color to our immune response. But this blueprint doesn’t represent the finished article. It’s the interpretation, regulation, and practical adjustments to our DNA that determine what our bodies ultimately look like and how they function, including the expression of diseases. These elements are controlled by the other three ‘omes.
For proteins to be made, the genome must first be read and copied onto messenger ribonucleic acid (mRNA) molecules. This process of transcription results in the transcriptome – the total mRNA molecules present, which describes the genes that are active and being expressed at particular moments. An mRNA sequence should mirror the sequence of the DNA blueprint from which it was transcribed. However, sometimes abnormalities in the transcriptome can alter the types and quantities of produced proteins, which can lead to disease development or progression.
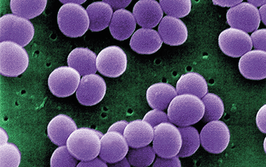
The methylome refers to a chemical modification where methyl groups are added to the DNA strand. Methylation is an epigenetic change, meaning it does not alter the underlying DNA code/genome but influences how and when genes are expressed. For example, a methyl group might silence tumor suppressor genes, which normally act to prevent cancer by controlling cell growth and repairing DNA damage. Since methyl groups do not directly change the DNA strand, it would be challenging to spot signs of cancer by only looking at the genome until physical tumors formed.
DNA is stored in a highly complex structure called chromatin. It’s possible for epigenetic changes to alter chromatin structure and affect how tightly DNA is packaged. This packaging determines the accessibility for turning genes on and off – abnormal packing can lead to inappropriate gene expression. For instance, tight packaging might prevent genes necessary for normal cell function from being expressed. Conversely, loose packaging can result in the overexpression of certain genes, which can contribute to conditions like autoimmune diseases or developmental disorders.
The multi-ome in practice
The complex layering of the four ‘omes demonstrates that there are plenty of points where biology can go awry between the genome’s original plan and final expression. A groundbreaking study from the University of Washington, USA, demonstrated the effects of the multi-ome in practice, by sequencing all four simultaneously to understand a patient’s expressed symptoms (3).
The study focused on an undiagnosed nine-month-old female with several unexplained phenotypes, including bilateral retinoblastomas, developmental delay, polymicrogyria, sensorineural hearing loss (SNHL), lactic acidosis, hypotonia, and dysmorphic facial features. University of Washington researchers used the latest single-molecule real-time (SMRT) sequencing methods to produce data that showed how each ‘ome explained the molecular basis for different symptoms.
For example, the patient’s developmental delay could be identified through the genome, caused by NBEA haploinsufficiency – when one of the two NBEA genes is missing or faulty. However, her bilateral retinoblastomas were caused by chromatin epigenetic change, specifically the deactivation of the RB1 cancer suppression gene. Since the change did not impact the DNA sequence, it could not have been identified by only analyzing the genome.
In the past, multi-omic approaches to complex disease studies have been hindered by the requirement of multiple assays, sequencing runs, technologies, and combining separate datasets. However, advancements in sequencing technology are making it possible to gain insights into all four ‘omes in a single experiment, with increased accuracy and lower cost, as demonstrated by researchers at the University of Washington. The increased depth and breadth of insights made available by the multi-ome will bring hope for those patients who cannot access answers after genomic analysis alone.
Though demonstrated here for a human genome, a multi-omic approach can be applied to any biological sample to gain a deeper understanding of its molecular fabric. There are huge opportunities for complex plant genomes and population genomics in biodiversity that can drive research breakthroughs in other important areas, such as food production and animal health.
- S Nurk et al., Science, 376, 6588 (2022). DOI: 10.1126/science.abj6987.
- K Ibañez et al., Lancet Neurol, 21, 3 (2022). DOI: 10.1016/S1474-4422(21)00462-2.
- MR Vollger et al., bioRxiv (2023). DOI: 10.1101/2023.09.26.559521.
Chief Operating Officer, PacBio