IPSSO Facto
Proceedings from the 12th Arkadi M. Rywlin International Symposium in Anatomic Pathology

The Arkadi M. Rywlin International Pathology Slide Seminar Organization (IPSSO) is pleased to announce the release of the proceedings from the 12th Arkadi M. Rywlin International Symposium in Anatomic Pathology. Held in Venice, Italy, during May 22–24, 2023, this symposium marked another milestone in the organization’s commitment to fostering collaboration and knowledge exchange among pathologists worldwide.
The Arkadi M. Rywlin IPSSO was founded in 1990 as a nonprofit entity with the primary goal of facilitating the sharing of ideas and histopathology slides among its members. Today, the organization has evolved into a vibrant community of over 50 like-minded professionals from countries across Europe and the Americas, who are all dedicated to advancing the field of pathology.
The inspiration behind the formation of this IPSSO lies in the legacy of Arkadi M. Rywlin, professor of pathology at the University of Miami School of Medicine and chairman of the Pathology Department at the Mount Sinai Medical Center of Greater Miami. Renowned for his commitment to free-thinking pathology, Rywlin’s influence continues to resonate within the organization, driving its members to pursue excellence in their work.
This symposium’s proceedings hold particular significance as they are dedicated to the memory of Ondřej Hes – a member of the organization who sadly passed away in July 2022. Hes, a professor of pathology at the Charles University in Pilsen, Czech Republic, made significant contributions to the field, particularly in the study of kidney tumors. His expertise and generosity of spirit left an indelible mark on his colleagues, and he will be fondly remembered for his invaluable contributions to the organization and the broader pathology community.
The Arkadi M. Rywlin IPSSO extends its gratitude to all those who contributed to the success of the symposium, including The Pathologist team for publishing the cases, digital pathology platform Pathcore for hosting them, and Ivan Damjanov, Emeritus Professor of Pathology at the University of Kansas School of Medicine, USA, for his unwavering support.
Special thanks are also extended to the University of Modena and Reggio-Emilia, and the organizing committee, especially to Irene Gullo from the São João Hospital Center, Faculty of Medicine, and Miguel Carneiro from the Centro de Investigação em Biodiversidade e Recursos Genéticos (CIBIO), both at University of Porto, Porto, Portugal, for their efforts in hosting the event.
Finally, thanks to every member of the Arkadi M. Rywlin IPSSO for their invaluable contributions to this endeavor and for their commitment and altruistic engagement.
For the detailed presentation, analysis, and references for each case, please download the case handout.
Click on the thumbnail images below to access the interactive whole-slide images for each case. For the detailed presentation, analysis, and references for each case, please download the case handout.
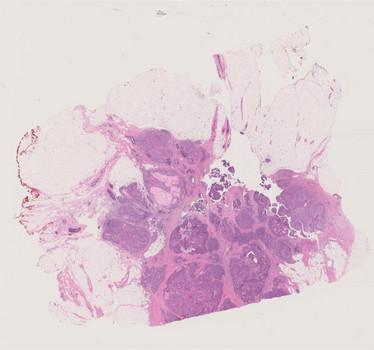
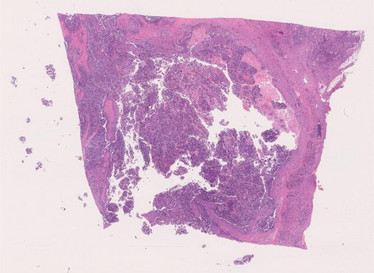
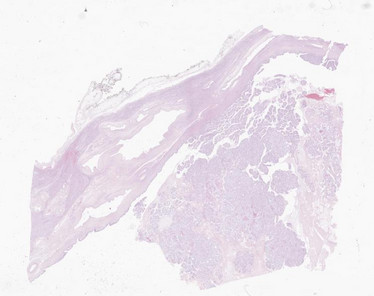
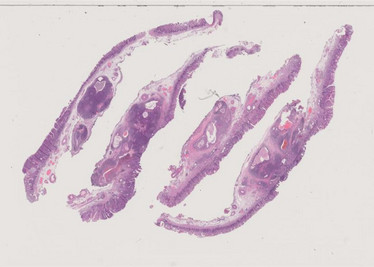
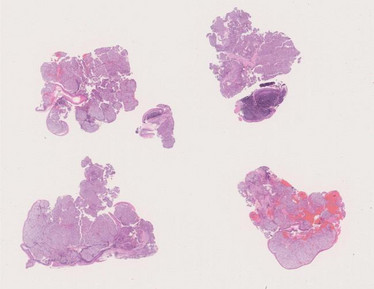
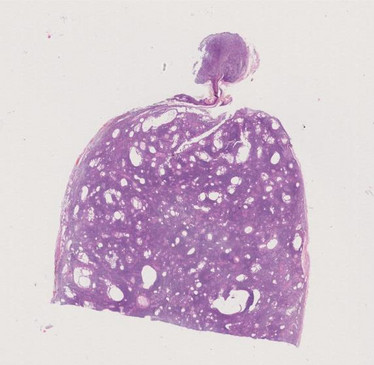
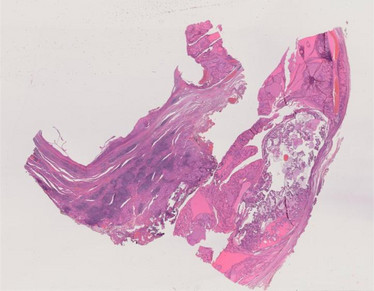
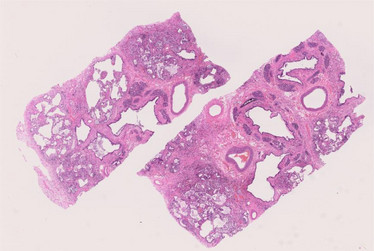
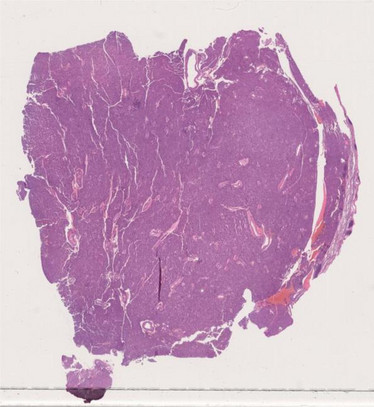
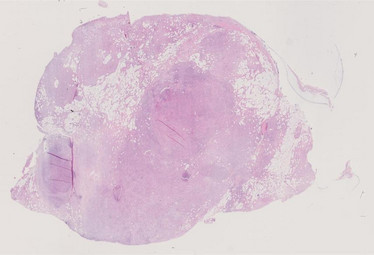
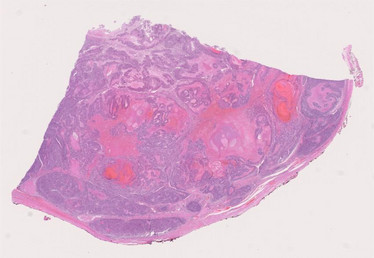
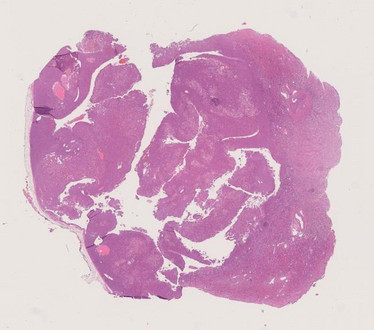
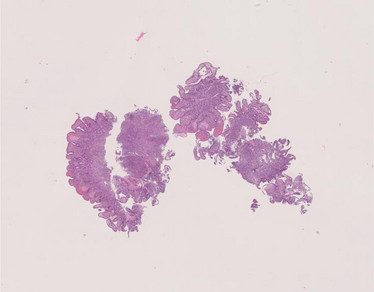
1. A 68-year-old woman presented with a spiculated left breast mass found on screening mammography. The lesion was biopsied and excised. The slides are from the excision.
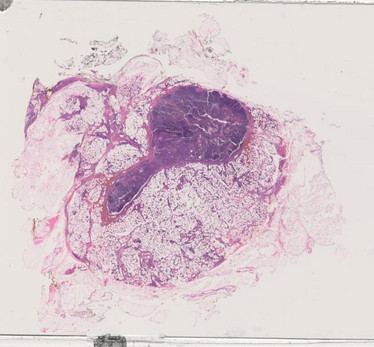
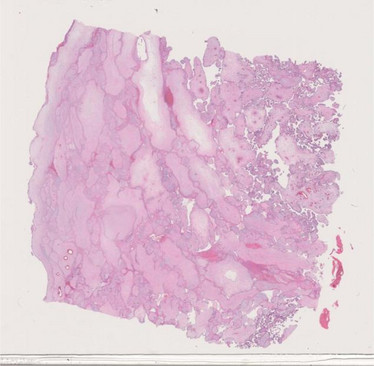
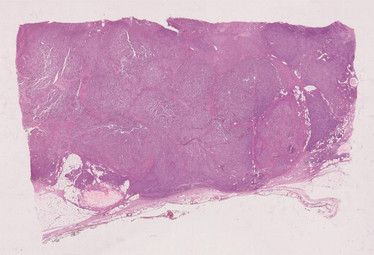
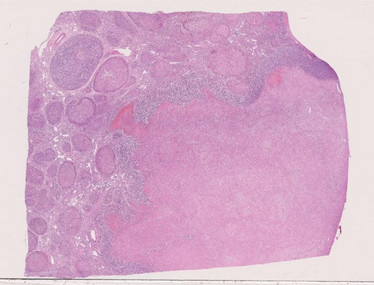
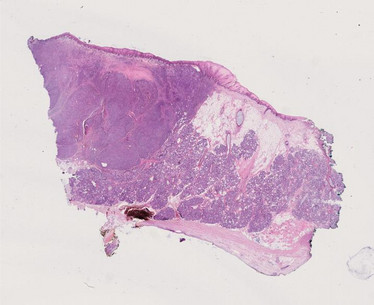
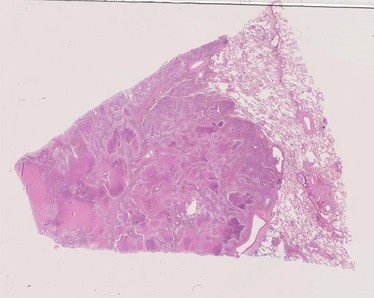
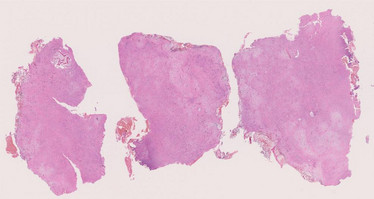
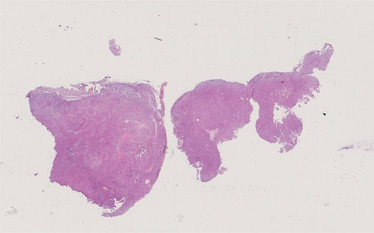
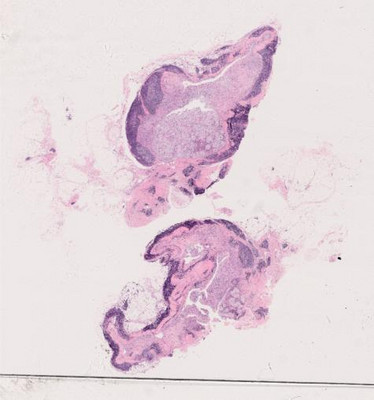
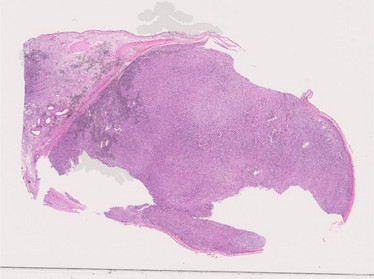
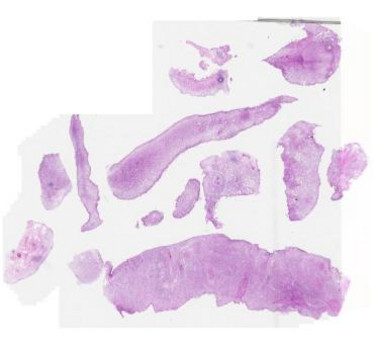
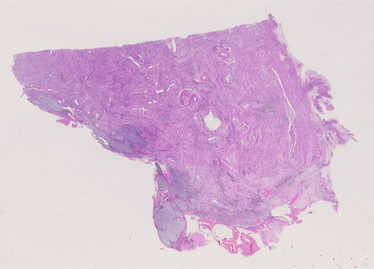
2. A 70-year-old female presented with recurrent right axillary adenopathy. The slides are from a limited axillary dissection.
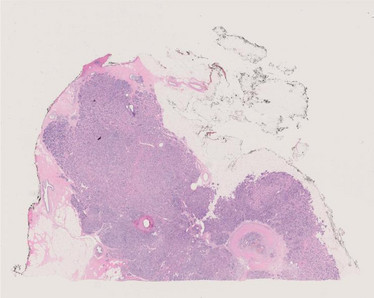
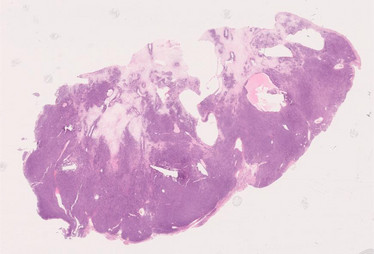
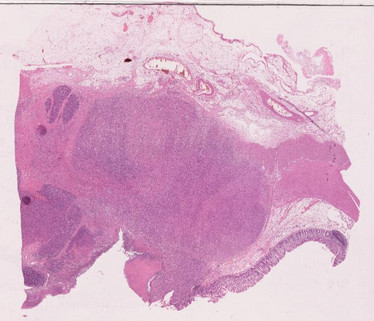
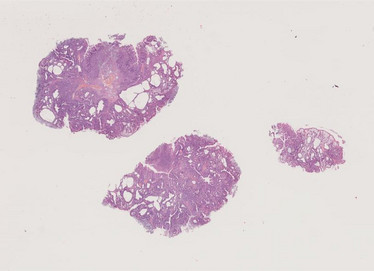
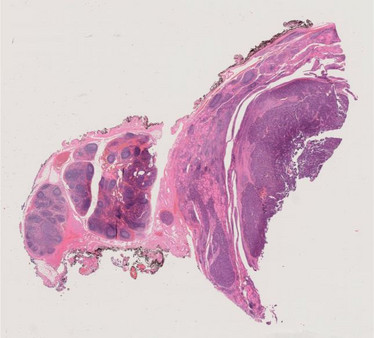
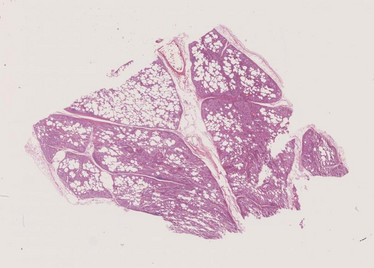
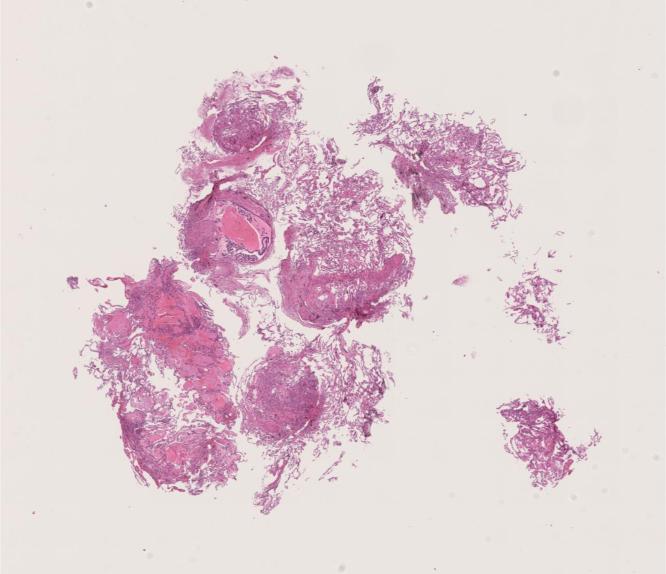
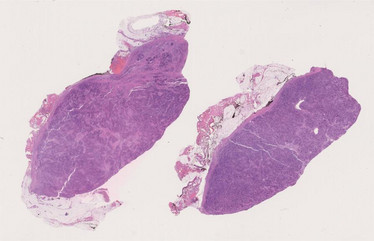
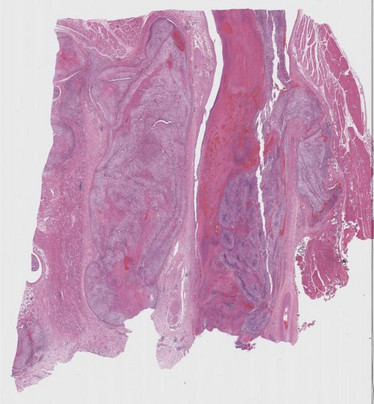
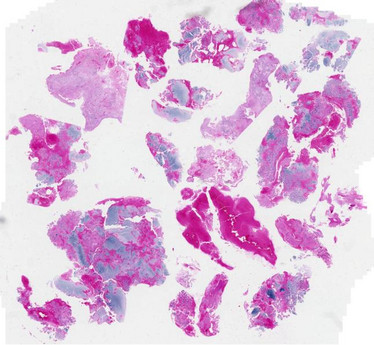
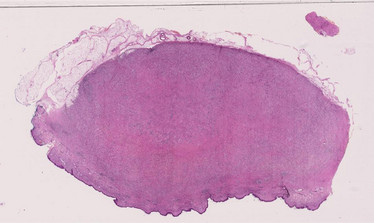
3. A 61 yrs. old woman presented with a 2 cm nodule located in the UOQ of the right breast. A core needle biopsy was performed resulting in a B3 lesion. At the multidisciplinary meeting a decision to remove the nodule was taken. After surgical removal of the lesions, the patient was follow-up with mammography every year. Seven years after surgery, microcalcifications appeared on the UOQ of the right breast, in strict connection with the surgical scar. After the diagnosis of high grade duct in situ carcinoma (DCIS), performed on vacuum assisted biopsy, surgical resection with clear margins was performed; the sentinel node biopsy was negative. The surgical resection evidenced invasive carcinoma, no special type (NST), grade 2, associated with high grade DCIS and lobular in situ carcinoma (LCIS). The patient, followed up with annual mammography, is presently alive with no evidence of disease.
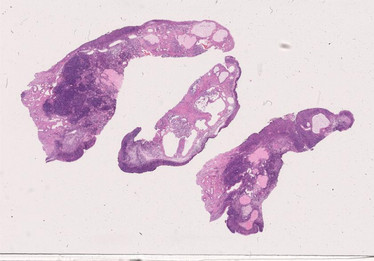
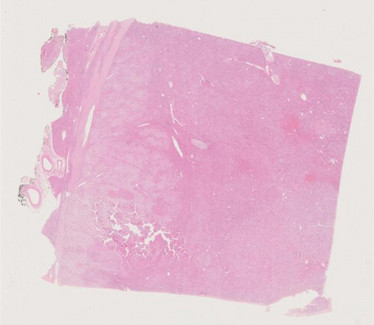
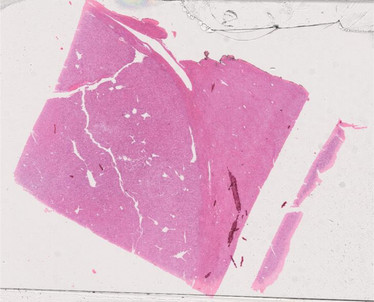
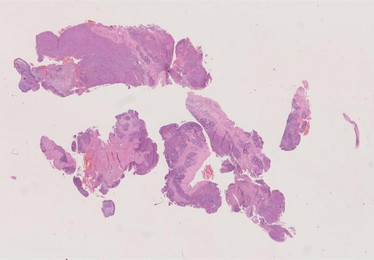
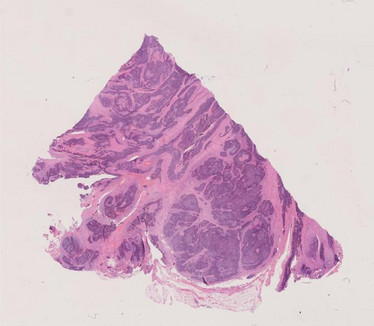
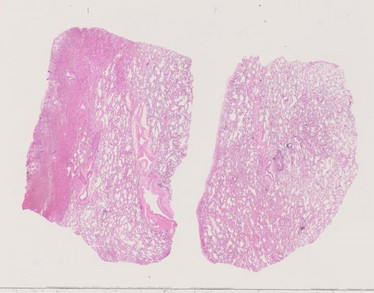
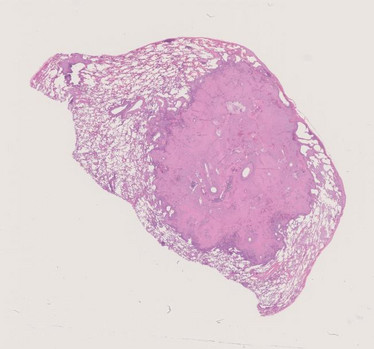
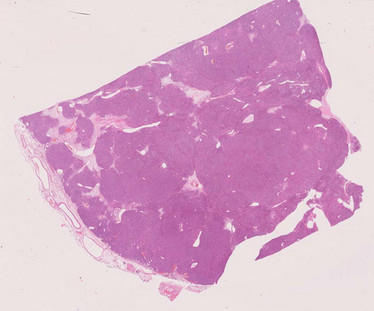
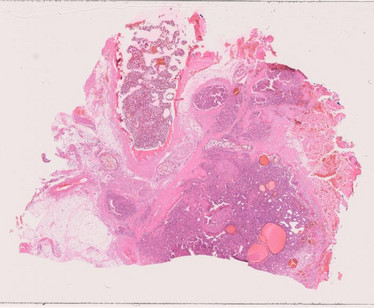
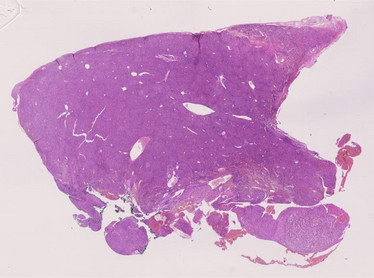
4. A 54-year-old, G1P1, female was admitted with a six-month history of abnormal uterine bleeding. She had no history of malignancy. Image analyses indicated an endometrial tumor in the fundus. Cervical and endometrial cytology showed "adenocarcinoma" (high grade serous or endometrioid carcinoma, grade 3, suggested) Endometrioid biopsy indicated a high grade endometrial carcinoma. A total abdominal hysterectomy, bilateral salpingo-oophorectomy and pelvic lymph nodes dissection was scheduled but declined by the patient and her family. She has not visited our hospital again so far.
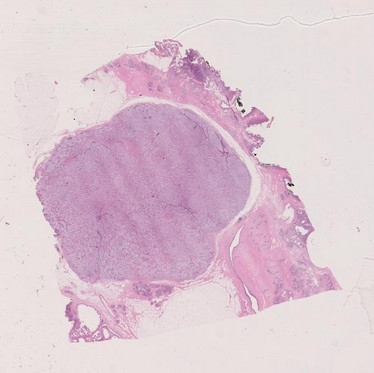
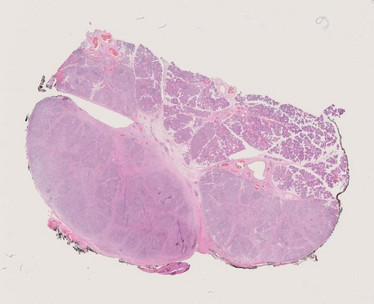
5. A 48-year-old woman presented with a 4 cm mass in the upper pole of the left kidney, 11 cm left adnexal simple cyst, and a 2.3 cm solid mass in the right ovary. The patient underwent partial nephrectomy for clinical-radiologic concern for clear cell renal cell carcinoma, and right salpingo-oophorectomy for the solid right ovarian mass. Frozen section evaluation of the right ovarian mass was diagnosed as metastatic renal cell carcinoma.
6. A 54-year-old woman presented a 2 cm nodule located in the IUQ of the right breast, classified on ultrasound as U3. After a core needle biopsy diagnosed as B3, the nodule was removed. After the diagnosis of benign lesion, the patient did not receive any further therapy. Four years later she presented a second nodule located in the UOQ of the right breast, that was histologically diagnosed as fibroadenoma. The present, presently followed-up in the local breast screening program, does not present any further breast lesion.
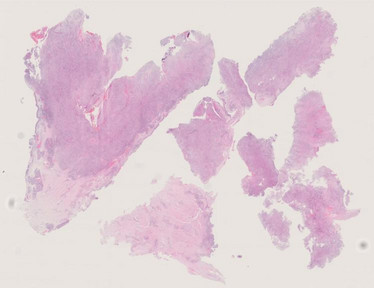
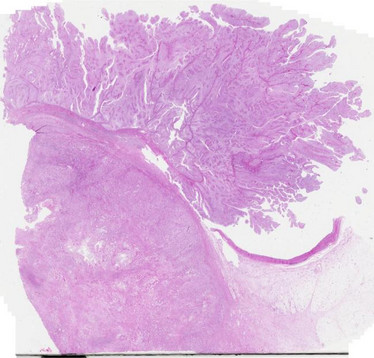
7. A 25-year-old, GOPO, female was admitted because of abnormal uterine bleeding. A diagnosis of endometrial curettage in other hospital was carcinosarcoma and a total hysterectomy and chemotherapy were considered. The patient visited our hospital for asking a second opinion and a conservative treatment. On the review of the slide, a diagnosis of corded and hyalinized endometrioid carcinoma was rendered and hormonal (medroxyprogesterone acetate, MPA) therapy has been performed. She is well without recurrent four years after the therapy.
8. A 36-year-old female with a history of advanced stage ovarian tumor, status-post bilateral salpingo-oophorectomy, omentectomy and tumor debulking, adjuvant chemotherapy (4 cycles of BEP), and on maintenance treatment with Arimidex, was found to have progression of her residual abdomino-pelvic disease on a follow-up visit. At that time, she also reported abdominal pain and nausea. Of note, the initial diagnosis had been rendered 7 years earlier and although the patient had had some residual disease, this had remained stable and she had been asymptomatic. Her last imaging studies showed nodules of variable size, the largest measuring several cm and located in the left upper quadrant. The patient underwent partial tumor debulking and resection of the transverse colon. Then, she was placed on a temozolomide trial.
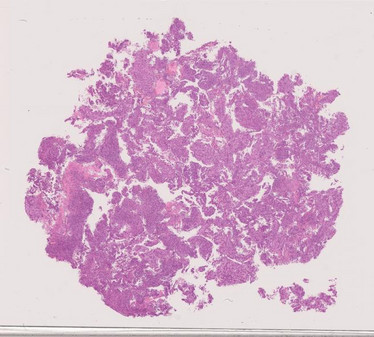
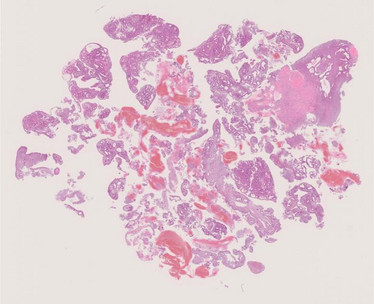
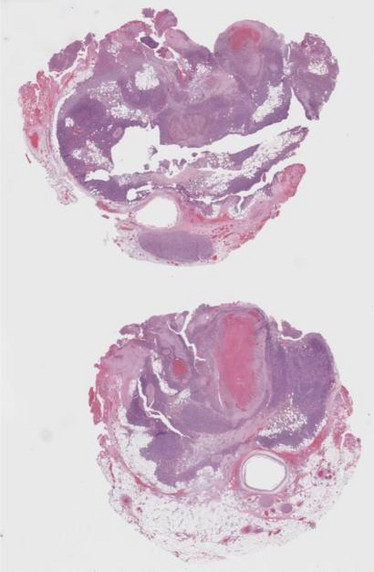
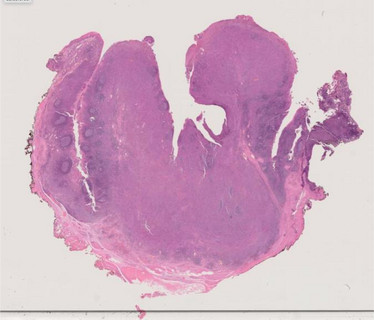
9. A 22-year-old woman with two prior pregnancies (one resulting in a first trimester abortion, and the second resulting in intrauterine fetal demise at 26 weeks gestation), presented at 34 weeks and 6 days gestation by ultrasound with decreased to absent fetal movements for the prior 8 hours. Ultrasound performed in the emergency department was consistent with intrauterine fetal demise. The pregnancy had been complicated by abnormal placental ultrasound findings, most notably an area concerning for a large chorangioma, and severe fetal growth restriction. Additional differential diagnosis from a radiologic perspective included a twin gestation with a partial hydatidiform mole component. The patient underwent induction of labor and vaginal delivery. Fetal autopsy was significant for a slightly small fetus for gestational age, without other overt gross or microscopic abnormalities.
10. A 32-year-old female presented to the emergency room with acute abdomen. Imaging studies showed a 15.0 cm right ovarian mass. Her serum CA125 was 500 U/mL. She underwent a TAHBSO and staging.

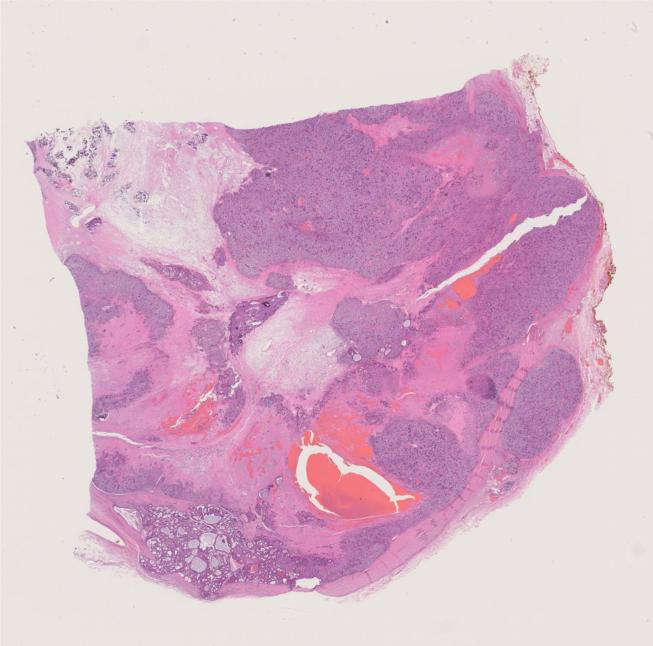
11. A 47 year-old man presented with epigastric pain and underwent abdominal ultrasound that disclosed a 6 cm mass in the liver, along with multiple smaller liver lesions. A needle core biopsy of the liver mass was performed (the scanned slide of this biopsy is available online), which was diagnosed as hepatocellular carcinoma in the outside institution. The patient was referred to our hospital to be evaluated for a liver transplantation. We re-reviewed the outside biopsy and came to different interpretation which led to more detailed analysis including MR and DOTA-PET scans which also disclosed a portal vein thrombosis and a pancreatic lesion. Based on the revised diagnosis, the patient underwent lutetium therapy followed by the post-neoadjuvant resection of the main liver mass, along with resection/ablation of smaller liver tumors, resection of portal vein thrombus and distal pancreatectomy (represented in the resection slides that were submitted for your review).
12. Female, 30-year-old. History of oral contraceptive. A US performed during a check-up for renal colic revealed two lesions in the liver, the major > 5 cm.
Imaging (PET; CT; MNR) suggestive for hepatocellular adenoma.
CEA, Ca19.9, NSE: negative.
Pre-operative diagnosis: hepatocellular adenoma.
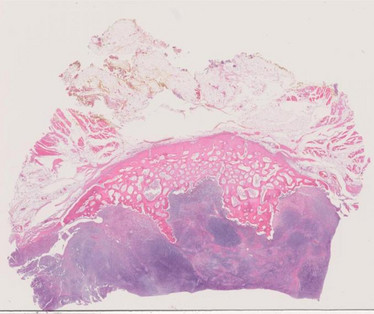
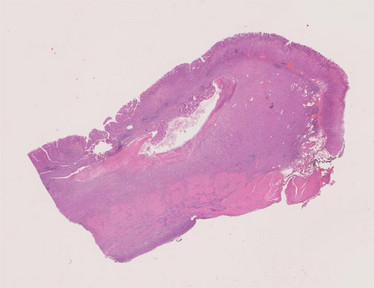
13. A 70 year-old man with hypertension and diabetes presented with progressively increasing malaise in the last six months. Serologic tests were unremarkable other than increased C-reactive protein. When his symptoms and signs did not subside, he eventually underwent more detailed analysis involving abdominal MRI disclosing a complex cystic lesion with a differential diagnosis of "cystadenocarcinoma" or a hydatid cyst. The patient underwent left hepatectomy that revealed a 12x9x6 cm relatively demarcated partially cystic and partially solid mass. The tumor also displayed intraductal growth.
14. A 53-year-old man without other relevant previous clinical history presented with new-onset symptoms and clinical signs of Cushing disease. Biochemical investigations recalled highly elevated serum cortisol and ACTH, but CRH was very low. With a subsumption of probable ACTH-producing pituitary adenoma, imaging studies were performed but failed to show any abnormalities in the Sella turcica or the surrounding organs, so that genuine or ectopic pituitary adenoma could be ruled out. An abdominal and thorax CT was performed which revealed no intrathoracic lesions. The adrenal glands appeared diffusely enlarged without mass-forming lesions. However, the pancreas showed a large contrast-enhancing mass occupying most of the head and body measuring 8 cm in maximum diameter. Coe needle biopsies revealed differentiated neuroendocrine neoplasm with Ki67 index >20%. Immunohistochemistry confirmed expression of ACTH in the neoplastic cells as the origin of the ACTH.
15. A 46-year-old man underwent heart transplantation for dilatative cardiomyopathy 6 years ago. He has been under regular monitoring without signs of transplant rejection. Currently, he presented with abdominal pain and fatigue. Hemoccult test was positive. Upper Gl endoscopy was unremarkable, but colonoscopy revealed multiple polypoid lesions in the left colon measuring up to 8 mm in size with variable superficial ulcerations. Abdominal CT showed in addition multiple liver nodules measuring up to 3.5 cm. Core needle biopsies was obtained from a liver lesion, followed then by left hemicolectomy and partial hepatectomy. No additional findings in other organs were seen on further imaging.
16. Female, 55-year-old. Previous lipoma of the breast. A US performed during a check-up for abdominal pain revealed a 5 cm lesion in the liver. Imaging (PET; CT; MNR) negative for other lesions. CEA and alfa-fetoprotein: negative; Ca 19.9: 69 U/ml. Pre-operative diagnosis: hepatocellular carcinoma.
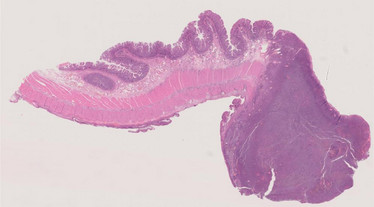
17. A 70-year-old male underwent endoscopic submucosal dissection for a subcardic 3cm lesion (type Ila+ls). Previous history of acute myocardial infarction and epidermoid carcinoma of vocal cord, removed by surgery 4 months before.
18. A 62-year-old man with a history of non-alcoholic steatohepatitis-associated cirrhosis was found to have two enlarging LI-RADs 5 lesions in the liver on routine screening for hepatocellular carcinoma. A biopsy of one of the masses was performed, and following the diagnosis, liver transplantation was performed within 2 weeks.
19. A 38-year-old male underwent total gastrectomy for multiple polyps in the body/fundus of the stomach.

20. A 59-year-old man with recent COVID-19 infection presented with gastrointestinal symptoms including diarrhea, anorexia, nausea, and weight loss (approximately 90 Ibs.). He also noted hyperpigmentation on his hands.
21. A 66-year-old man presented with a tumor of the nasal cavity, that was originally diagnosed as high grade squamous cell carcinoma. The new excision was performed at another hospital with diagnosis of acinic carcinoma with high-grade transformation. Due to an uncertain diagnosis, the tumor was sent to us for second opinion. Six months after primary excision, the patient presented with huge recurrent tumor in the nasal cavity, with a cervical lymph node metastasis. The patient died 10 months after primary surgery having been treated by chemotherapy.
22. A 51-year-old Chinese male, ex-smoker with G6PD, presented with a painless base of tongue tongue lesion which had bled for 2 days. On clinical examination, a tumor was seen located to BOT/lateral pharyngeal wall. An MRI-study was performed and showed a 5 cm tumor in the left lateral oro-pharyngeal wall, centred in the parapharyngeal space. A PET -CT was negative for distant spread. An incision biopsy was done. The tumor was resected at another hospital, where also a repeat biopsy was performed (showing the same features as in the first biopsy specimen). The resected specimen contained a 5.2 cm tumor which displayed the same histological features as in the biopsies. No necrosis, HGT or PNI was seen, but focal LVI was present. All margins were negative (7-18 mm). Bilateral modified neck dissections revealed no LN metastasis.
23. A 69-year-old man presented with a tumor of the left parotid gland. The tumor measured 50x45 mm, it had a solid consistency and whitish color. After resection, the patient had paresis of nervus facialis on the left side. Postoperative irradiation of the parotideal area and neck on the left was administered with a total dose of 60 Gy in 30 fractions. The radiotherapy was completed in December 2022 and the patient is now without any oncological treatment. On the last check from 2/2/2023 he was without evidence of disease.
24. An 81-year-old man with epistaxis since 1.5 years. Previous history of gastric DLCBCL 14 years previously. CT H&N revealed a 3x4.2x5 cm sized destructive sinonasal lesion interpreted as malignant tumor. First, a biopsy was taken and later tumor reducing curettage was performed.
25. A 75-year-old woman (history of hypothyroidism and rheumatoid arthritis) presented with a large neck mass originating from anterior inferior parotid gland that had been present for 10 years. It has increased in the last 8 months with occasional pain. Ultrasound showed a 3 cm nodule in parotid gland with calcifications. Core needle biopsy showed fibrous tissue with aggregates of atypical glandular epithelium. She underwent L superficial parotidectomy, facial nerve preservation, and selective neck dissection. She is without evidence of disease 1 year later.
26. A 41-year-old man presented with a tumor of the parotid gland.
27. A 36-year-old female presented with a tumor of the soft palate.
28. A 19-year-old female presented with an incidental finding of a palpable mass in the left lobe of the thyroid gland. She had no relevant past medical history. Her family history, however, included a sister with rhabdomyosarcoma at age of 19, a maternal cousin with Wilms' tumor at age 5, and a history of papillary thyroid carcinoma and breast cancer in other family members. The patient's paternal family history also included breast and pancreatic cancer. On physical examination, the patient had neck swelling with intermittent difficulty swallowing. She was referred by her clinician for ultrasonography. The ultrasound demonstrated a dominant, solid, mildly left-sided nodule with increased vascularity that nearly replaced the left thyroid lobe, and measured 4.9 x 3.3 x 5.9 cm. The mass at the base of the left thyroid lobe deviated the trachea to the right and partially narrowed it. Two weeks later, a follow-up CT of the neck with intravenous contrast showed a slight increase in size to 5.1×4.7x6.1 cm without definite evidence of extension beyond the thyroid surface or substernal extension.
29. An 85-year-old man with fatigue. Previous history of idiopathic membranous glomerulonephritis in1992, prostatic adenocarcinoma Gleason 3+4=7 in 2003, polyarthritis in 2008, and multiple skin basal cell carcinomas now presenting with a left sided neck lump in region Ib. Radiology revealed a 36 mm sized expansile tumor in submandibular gland. FNA performed but was non-informative due to lack of diagnostic material. A core needle was later performed under clinical suspicion of malignancy but the pathological interpretation was rather inconclusive since both a reactive inflammatory condition and a biphasic salivary gland tumor of uncertain malignant potential (SUMP) could be discussed. Left glandula submandibularis with tumor was resected for histopathological examination.
30. A 20-year-old female discovered to have a 5.0cm left thyroid nodule in 2019. Prior biopsy: 11/12/2019: Follicular Lesion of Undetermined Significance - FLUS (Bethesda Category Ill) In 2022, then 23-year-old female with a left thyroid nodule has been needled as Thyroseq benign but is nearly 8 cm. CT scan and ultrasound showed a large mixed cystic and solid nodule replacing the left lobe of the thyroid gland with shift of the trachea to the right but no substernal extension. No definite suspicious cervical lymph nodes. US thyroid performed in October 2022 showed a 7.7cm mixed cystic and solid nodule replaces the majority of the left thyroid lobe. No right thyroid nodules identified. Heterogeneous thyroid parenchyma suggestive of changes of Hashimoto thyroiditis. Mother with history of papillary thyroid carcinoma.
31. A 75-year-old man with no significant past medical history was seen for symptoms of persistent cough. CT scans showed a mass involving the right upper lobe of lung. Following a core needle biopsy, the patient was scheduled for surgery. A thoracotomy with right upper lobectomy was performed. The gross specimen showed a large subpleural mass that measured 5.4 x 4.5 × 3.0 cm. The regional lymph nodes were all free of tumor.
32. A 33-year-old previously healthy woman presented with exertional dyspnoea and non-productive cough, which she reported following the exposure to the smokes of a fire. No other risk factors for lung disease nor systemic symptoms were present. Laboratory parameters were normal except for mild thrombocytopenia. Pulmonary function tests revealed a restrictive pattern, and HRCT of the chest showed bilateral ground-glass opacities with focal thickening of interlobular septa. A bronchoscopy with bronchoalveolar lavage (BAL) and transbronchial biopsy (TBB) was performed: both showed only foamy macrophages and were considered non diagnostic, so a video-assisted thoracoscopic biopsy was obtained (the material you received).
33. The patient is a 29 y.o. male with a history of cystic fibrosis, diabetes, and chronic respiratory failure requiring bilateral orthotopic lung transplantation at another institution, approximately 3 years prior to current admission. He had several post-operative episodes of acute cellular rejection, and an episode of right pneumothorax after a transbronchial lung biopsy; it required chest tube placement. Approximately 1 years after transplantation, he developed progressive dyspnea on exertion and severe gastroenteric reflux disease (GERD). The forced expiratory volume at 1 second (FEV1) decreased more than 10% predicted to 60% predicted and he was diagnosed with bronchiolitis obliterative syndrome (BOS). This diagnosis requires an FEV1 <75% predicted, an irreversible ≥10% decline in FEV1 <2 years, a FEV1-to- vital capacity (VC) ratio <0.7 or the lower limit of the 90% confidence interval of the ratio, absence of infection, and a preexisting diagnosis of chronic graft versus host disease or of air trapping on physical examination and imaging studies.
34. The patient is a 67 y.o. male who developed COVID-19 syndrome with fever, congestion, body aches and cough about 2 ½ years prior to this admission. He was overweight and had no previous preexistent illnesses such as diabetes, hypertension, or others. The respiratory symptoms worsened, and he developed progressive dyspnea that required hospitalization to a respiratory intensive care unit (RICU). On admission, he was diagnosed with respiratory failure and bilateral pneumonia. Imaging studies showed extensive bilateral pulmonary infiltrates. He was intubated and treated with antibiotics, steroids, and other medications. He was extubated after several weeks in the RICU and discharged with a diagnosis of chronic respiratory failure on 5-6 liters of oxygen. He remained extremely dyspneic and was unable to climb one flight of stairs. The respiratory insufficiency worsened, and lung transplantation was recommended.
35. A 62-year-old man was found to have a large mass in the left lung and multiple bony metastases. A biopsy of the lung mass was obtained, and this showed a poorly differentiated malignancy with features diagnostic of NUT carcinoma. IHC for NUT was diffusely positive with a speckled nuclear pattern; diffuse expression of p40 was also present, along with patchy staining for AE1/AE3 and Cam5.2, without staining for TTF-1, SOX10, CD34, CD45, or S100 protein, and normal (retained) expression of INI1 and BRG1. Next-generation sequencing confirmed the presence of a BRD3- NUTM1 fusion. The patient received multiple cycles of palliative chemotherapy with carboplatin and paclitaxel and radiation to his spine and hip. Because of severe hip pain from a large metastatic tumor deposit in his pelvis and an impending pathologic fracture, a resection and reconstruction of the right hemipelvis was performed.
36. A 76-year-old previously healthy man presented with cough and mild fever persisting for more than 1 month. Blood exam showed an increase in inflammatory markers and neutrophilia, with negative autoimmune and oncologic markers. At CT-scan multiple nodules were present in both lungs, some of them cavitating and associated with minimal ground-glass opacities: the radiologic differential diagnosis was metastases, septic emboli/infection and granulomatosis with polyangiitis (Wegener's granulomatosis). A percutaneous fine-needle biopsy was performed, showing suppurative inflammation with negative culture results. A bronchoscopy with bronchoalveolar lavage (BAL) and transbronchial biopsy (TBB) was obtained: BAL was negative, whereas TBB was the material you received.
37. A 33-year-old woman with end-stage renal disease of unclear etiology at age 18 and prior renal transplantation at age 22 was found to have numerous bilateral pulmonary nodules. After a biopsy performed at an outside hospital was non- diagnostic, the patient underwent a wedge resection of one of the lung nodules.
38. A 43-year-old man with chest pain and dyspnea. Imaging shows an intrapulmonar mass. Lobectomy was performed.
39. A 47-year-old man presented with pulmonary and brain metastases of a tumor that had presented initially 9 years prior in the pelvis and was then diagnosed at the time as a clear cell malignant tumor of unknown origin.
40. A 58 year-old woman with chest pain. Imaging shows an anterior mediastinal mass. Surgical resection via thoracotomy was performed.
41. A 63-year-old man was seen in the clinic for back pain and abdominal discomfort. CT scan of the abdomen revealed a large retroperitoneal mass. The patient's past history was significant for a hernia operation and cataract surgery. An en-block resection was scheduled. At surgery, the mass was unencapsulated but well circumscribed and attached to the colon. It showed a smooth outer surface with a small amount of attached adipose tissue and measured 15 x 13 x 10.9 cm. The cut surface was tan-pink and homogeneous, with focal areas of softening. The segment of colon was unremarkable.
42. A 55-year-old man presented with a sharply circumscribed right inguinal tumor sized 4 x 3 x 2 cm (Fig. 1) which was excised. The patient was without signs of metastatic disease at presentation
43. A 75-year-old female with a history of rheumatoid arthritis presented to an orthopedic clinic with a mass at the base of the left ring finger. An MRI identified a T2 hyperintense mass with an irregular margin measuring 1.2 cm in greatest dimension in the palmar and radial aspect of the left fourth finger. Ultrasound also noted a complex cystic lesion at the anterior base of the left fourth digit with thick vascular septations that would be atypical for a ganglion cyst. During the procedure, the surgeon excised the lesion, which was clinically felt to be compatible with a retinacular cyst emanating from the flexor sheath.
44. A 72-year-old female presented with a 6.5 cm soft tissue mass in the left thigh infiltrating the femur.
45. A 21-year-old woman with no significant past medical or surgical history was found to have a large pelvic mass during routine annual gynecologic examination. She noted urinary frequency, dysuria, constipation, abdominal fullness, and cold sweats. Pelvic ultrasound demonstrated a 14 x 10 x 11cm solid, vascular, central pelvic mass. Contrast-enhanced abdominal and pelvic magnetic resonance imaging (MRI) demonstrated a 15.7 x 13.5 x 11.8 cm heterogeneously enhancing pelvic mass of indeterminate origin with focal cystic change. The mass abutted the rectum and ovaries with inferior compression of the uterus and bladder. The uterus and ovaries were otherwise without abnormality, with the mass appearing separate from the uterus and ovaries. There was compression of the left ureter with secondary hydronephrosis. There was no adenopathy nor osseous abnormality. There was no evidence of metastatic disease within the chest or abdomen. Differential diagnostic considerations based on these imaging findings included gastrointestinal stromal tumor, exophytic uterine leiomyosarcoma, and primary peritoneal sarcoma. CT-guided biopsy was performed for definitive characterization.CT-guided biopsy was performed for definitive characterization.

46. A 58-year-old male presented with shoulder pain, right upper extremity weakness, and 15 lb weight loss was found to have a 7 cm soft tissue mass arising in his right teres minor muscle. A core needle biopsy was obtained (not shown) and a diagnosis was rendered leading to neoadjuvant chemotherapy (without significant clinical response - tumor had enlarged while on chemotherapy) thus prompting a wide surgical excision prior to completion of chemotherapy.

47. A 57-year-old male admitted to our hospital in Octuber 2017 for postoperative control of a soft tissue abdominal wall. The tumor was resected three times recurred twice in the last 20 years, in another institution, the last resection in June 2017. No recurrence was detected on admission.
48. A 53-year-old man presented with a 5 x 4.5 x 4 cm psoas muscle mass. He also had a large jejunal mass about 20 cm in maximum diameter. There was a history of HIV AIDS.
49. A 35-year-old female presented with a 7.5 x 5 x 2.5 cm periscapular mass. Patient had a history of neurofibromatosis 1.
50. A seven-year-old female with a 2 year history of left shoulder pain and microfractures in the proximal humerus. Radiography and CAT demonstrated an expansile osteolytic lesion involving the proximal metaphisis of the right humerus, with popcorn appearance (chondroid matrix).
51. A 30-year-old male presented with history of right middle back pain for 5 months. He also complained of right sided rib pain/discomfort and associated numbness.
52. A 46-year-old female presented with back pain, multiple fractures in different stages of healing, numerous bone lucencies, weakness, and paresthesias and an elevated Alkaline phosphatase. She had a recent M- spike on serum electrophoresis which led to a bone marrow biopsy showed a 0.4% monoclonal plasma cell population, IgA kappa-positive. Patient has a subsequent urine protein electrophoresis and urine immunofixation electrophoresis which did not show evidence of monoclonal gammopathy
53. A 22-year-old (otherwise healthy) male presented after experiencing a year of hip pain. He had no history of malignancy or radiation therapy. An MRI demonstrated a 13.4 cm mass in the left tensor fasciae latae muscle belly that was predominantly composed of fat. The mass had moderate heterogeneously enhancing central irregular soft tissue elements, radiologically interpreted as concerning for lipoma or atypical lipomatous tumor. During the procedure, the surgeon found the consistency of the mass to be unusual and questioned whether it could be necrotic. He decided to perform an incisional-type biopsy.
54. A 48-year-old man presented with a gradually increasing neck mass and 30 Ib. weight loss. He had intermittent dysphagia to liquids, associated cough and episodes of choking. CT scan from an outside hospital demonstrated a 2.5 × 2.4 x 2.4 cm. ovoid expansile mass limited to the left thyroid cartilage. The mass had radiologic features exhibiting chondroid matrix deposition. Radiologic impression was chondrosarcoma versus chondroma. The right thyroid cartilage and cricoid cartilage were radiologically unremarkable. Vertical hemilaryngectomy and left thyroplasty with tracheotomy was performed.
55. A 40-year-old woman presented with a central neck lump of 2 years duration that was progressively increasing in size. The patient had a subtotal thyroidectomy performed overseas 3 years ago for a tumor that was told to be benign. Clinical examination revealed a 2 cm hard, central neck mass that did not move on swallowing. A CT-scan of the neck showed a 1.9 cm, hyperdense, poorly circumscribed focus with irregular radiating tongue-like extensions in the central neck region. The patient initially underwent an FNA-biopsy (which was signed out as "a low-grade spindle cell neoplasm, likely of mesenchymal origin"), and the tumor was subsequently excised.
56. A 49-year-old woman with a 2.2 cm left renal mass.
57. A 69-year-old Mexican male, smoker for 50 years, one pack a day, complaints of pelvic pain and dysuria for 6 months. TAC with bladder mass and unilateral hydronephrosis.

58. A 59-year-old woman with a 1.8 cm right renal mass.
59. A 43-year-old female with urinary bleeding and loss of weight. CA19-9 and CA125 markers were negative.
60. A 71-year-old female patient developed an indurated lesion at the right hand. After a marginal excision a complete excision with tumour free margins had been performed and there is no sign of recurrence at 10 months.
61. A 44-year-old immunocompromised man performs a colonoscopy for suspected CMV colitis and a gastro- duodenoscopy because of severe pancytopenia. At gastro-duodenoscopy, the stomach appears distensible and the mucosa diffusely hyperemic, while starting from the duodenal bulb up to the third duodenal portion numerous, reddish-colored papules are seen, ranging in size from 2 to 10 mm. At colonoscopy all the tracts were in the normal range.
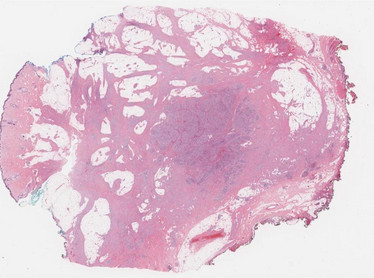
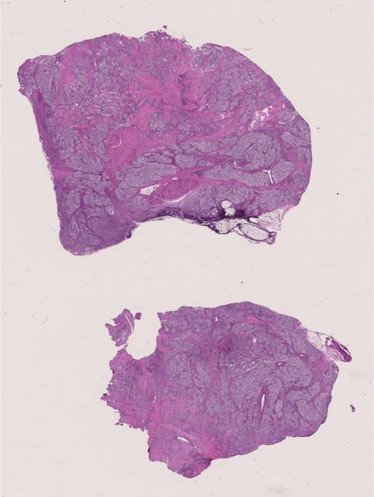
62. A 52 year-old female presented with uterine tumor. The myomectomy specimen was submitted for histology with a clinical diagnosis of uterine myoma. Malignant nature of the tumor was ascertained from the biopsy therefore hysterectomy with bilateral adnexectomy and resection of two additional tumor deposits from Douglas' space were performed.
63. An 87-year-old male patient complained about a fast-growing superficial tumour arising at the right elbow. After a biopsy a marginal excision had been performed and a 3.5 x 3.0 x 2.5 cm measuring lesion was described.
64. A 49-year-old female presented with abdominal discomfort which had been going on for more than two months. An abdominal computed tomography was performed which demonstrated a 3x2cm hypo-dense solid mass in lobus caudatus of the liver. The lesion was hypo-vascular and had an ill-defined border according to radiologist most probably hepatocellular carcinoma. Fine needle aspiration biopsy of the lesion was performed and diagnosed as metastasis of malignant melanoma. Because PET CT didn't show any other lesions, hepatic lesion was excised and sent for histology to our pathology department.
65. A 50-year-old male, with no significant past medical history, presented with left tonsil lesion.
66. A 75-year-old male, with no significant past medical history, presented with an acute abdomen and was found to have a small bowel perforation.
67. A 45-year-old HIV-infected patient had an initial gastroscopy for stomachache that revealed an ulcer at the level of the posterior wall of the gastric body. On the first biopsies the morphology, although immunohistochemical investigation with HHV8 was negative, suggested the diagnosis of Kaposi's Sarcoma. Abdominal CT scan after intravenous administration of contrast and after oral administration of water revealed focal thickening of the gastric wall at the level of the body-bottom passage of 37x25x10 cm. A partial gastrectomy was therefore performed.