Can we accept that meningothelial hyperplasia is a true preneoplastic proliferative, not a simple hyperplastic reactive, lesion, and is it time to change our approach to it? By Sanja M. Milenkovic, associate professor of Pathology and Oral Pathology at the Faculty of Dentistry, Pančevo, Serbia, and the chief of the Clinical Pathology Department, at the University Clinical Hospital Center Zemun, Belgrade.
The history of meningioma can be traced back to 1614, when Felix Paster first described the tumor, but it had not been officially named yet (1). It was Harvey Cushing who first coined the term “meningioma” in a monograph written with Louise Eisenhardt in 1938 (2). Where are we today? Well, knowledge of the condition is still lacking. When I ask radiologists to tell me how they might go about identifying meningioma, they might say: “Ok, I see a dural tail sing, it’s meningioma!” When I ask general pathologists what they know about the condition, there’s a good chance they would say, “Meningioma? It is a typically benign and slow growing tumor, appearing mostly in the later decades of life!”
But when I ask neuropathologists about meningiomas, they tend to be a lot more enthused: “Fascinating tumor …the wide-ranging biologic and histologic continuum of meningiomas has been impressive since the beginning of the 20th century…!” Thankfully, times have changed. Molecular pathology is here to stay, and over the course of the last century, scientific advancements have allowed us to identify many important facts about meningioma. We now know that the most common tumor suppressor genes associated with its development are NF2, DAL-1, and various tissue inhibitors of matrix metalloproteinases (TIMPs) (3,4). It’s great that we’ve amassed this knowledge. But have we forgotten meningothelial hyperplasia (MH)? “From the time when I was working on my PhD thesis in 2005 until now, there have only been a few articles about it, and even less that have attempted to define it.” What do we know? We know that it is most commonly diagnosed incidentally during surgery or at autopsy. We know in clinical practice, MH has been reportedly associated with advanced patient age, chronic renal failure, trauma, hemorrhage, and neoplasia (particularly prominent adjacent to optic nerve pilocytic astrocytomas, where it has the potential to be misdiagnosed as an orbital meningioma) (5).
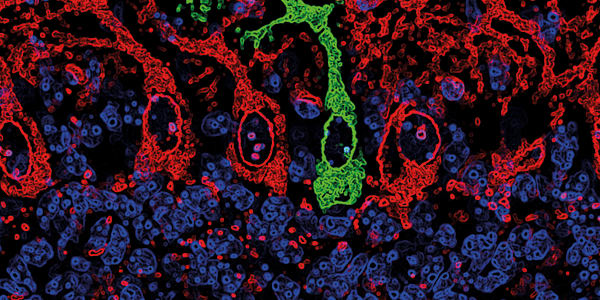
Overall, MH represents a poorly characterized entity and we continue to be challenged by it. In particular, as pathologists, we are faced with the following conundrums: 1) When small meningothelial nests are found within a submitted surgical sample, usually labeled as “dural margin”, it is really difficult to conclude if it is normal or hyperplastic meningothelial foci, or tumor spread. This is especially difficult if the meningioma radiologically shows dural tail sing; this sign histologically is nothing more than hypervascular fibrous tissue. 2) In rare cases, we have seen patients presenting with thin layers of meningeal enhancement of unknown etiology, where biopsy revealed thickened meninges with nests of arachnoidal cap cells. In these cases, it is very difficult to distinguish hyperplasia from “meningothelial tumorlets” or meningioma en plaque (5). MH is pretty incredible in nature; immunohistochemically it has a profile like normal arachnoidal cap cells, but with progesterone receptor (PR) positivity. On the other hand, we know that MH shows 64 percent similarity to meningiomas. We don’t see any deletions of NF2 or 4.1B by FISH analysis in MH, which we do see in classic meningiomas, and MH cells retain merlin and protein 4.1B expression (5). In a bid to shed some light, scientists have created a genetically engineered model, using conditional mutagenesis to specifically inactivate mouse Nf2 gene in arachnoidal cells and the results of these studies have confusingly shown formation of intracranial MH and meningiomas. The data suggests that MH may represent a preneoplastic lesion in some cases. To add further confusion, some important differences exist between the human and animal lesions. In humans MH is a reactive process, but in a mouse model (although the lesions are small), they are not reactive, but neoplastic (6). Is there a border between these two entities and if so, where is it? In my view, I think it’s better to talk about meningothelial proliferation in general, rather than MH specifically. And moving forward, I believe there is a need to develop additional studies and apply a rigorously controlled multidisciplinary approach to study this disease and, eventually, to define a suitable approach to its diagnosis and to its treatment. Until this time comes, the disease will be shrouded with question marks, uncertainty and, unfortunately, missed diagnoses.
References
- MG Netsky, J Lapresle, “The first account of a meningioma”, Bull Hist Med, 30, 465–468 (1956). H Cushing, L Eisenhardt, “Meningiomas: Their classification, regional behaviour, life history and surgical end results,” Bull Med Libr Assoc. 27, 185 (1938). M Shibuya, “Pathology and molecular genetics of meningioma: Recent advances”, Neurol Med Chir (Tokyo), 55, 14–27 (2015). PMID: 26236799. DH Gutmann et al., “Molecular biological determinations of meningioma progression and recurrence”, PLoS ONE, 9, e94987 (2014). PMID: 24722350. A Perry et al., “Meningothelial hyperplasia: A detailed clinicopathologic, immunohistochemical and genetic study of 11 cases”, Brain Pathol, 15, 109–115 (2005). PMID: 15912882. M Kalamarides et al., “Natural history of meningioma development in mice reveals: A synergy of Nf2 and p16Ink4a mutations,” Brain Pathol, 18, 62–70 (2008). PMID: 17924978.