Neuropathologists play a vital role in diagnosing complex diseases and neurodegenerative conditions that require a high degree of technical skill and specialized knowledge. Despite this, their contributions – and those of pathologists in general – are often undervalued within the broader healthcare system, particularly when it comes to reimbursement models. This undervaluation of pathology services not only affects the financial sustainability of labs but also directly impacts the quality of patient care.

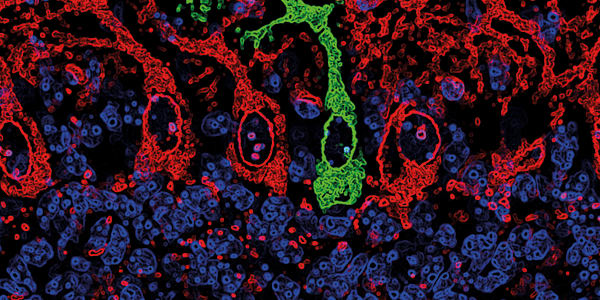
Credit: University of Texas Health Center
This issue is especially pressing in neuropathology, where diagnostic procedures, such as brain tumor biopsies, brain autopsies, amyloid and tau protein analyses, and cerebrospinal fluid testing, require significant expertise and advanced technology. Yet, these highly specialized services are frequently reimbursed at rates that fail to reflect the complexity and time required to perform them accurately. For example, both a complex brain tumor biopsy and a relatively simpler tubular adenoma are reimbursed under the same billing code, CPT 88305, which is designated for "Level IV Surgical pathology, gross and microscopic examination." Brain tumor biopsies understandably require far more time, technical expertise, and advanced diagnostic tools compared with a routine tubular adenoma gastrointestinal biopsy. Equal compensation for unequal work undermines the financial sustainability of neuropathology services, which depend on highly skilled labor and cutting-edge technology for accurate diagnoses.
Under the traditional fee-for-service model, pathologists are reimbursed based on the number of tests or procedures they perform. However, many essential diagnostic services in neuropathology, such as immunohistochemical staining for tumor classification or advanced molecular testing for brain tumor evaluations, are reimbursed at relatively low rates. This can be especially challenging for neuropathology laboratories that depend on high-cost, cutting-edge equipment to deliver precise diagnostic results. Moreover, fee-for-service models can incentivize higher testing volumes rather than prioritizing the accuracy and necessity of those tests – something particularly critical in neuropathology, where false positives or negatives can have serious clinical consequences.
The shift toward value-based care, while intended to improve outcomes and lower costs, presents additional challenges. Bundled payments – where services related to a particular treatment or condition are grouped together – further undervalue pathology services, including those provided by neuropathologists. This system puts undue pressure on lab leaders to reduce costs, which can limit their ability to invest in essential technology and training that keeps neuropathology at the forefront of patient care. One of the reasons for this undervaluation is the “invisibility” of much of the work performed by neuropathologists and pathologists overall. Unlike clinical specialties, where patient interaction is direct and visible, much of our work happens behind the scenes. This, combined with a lack of understanding of the complexity of neuropathological diagnoses, contributes to the misalignment between the value of our services and the compensation provided for them.
Addressing these reimbursement challenges requires a targeted, multifaceted approach. Advocacy efforts by professional organizations, such as the College of American Pathologists and the American Association of Neuropathologists, are essential to raise awareness among healthcare providers, insurers, and policymakers about the critical role of neuropathology in patient care. These organizations must also continue lobbying for reimbursement models that accurately reflect the value and expertise required in our field. Moreover, alternative payment models that better align incentives with the quality and outcomes of neuropathology services are urgently needed. Neuropathology-specific bundles that account for the complexity of individual diagnostic services could ensure fairer reimbursement, while quality-based models would better reflect the outcomes-driven focus of our work, particularly in the context of neurodegenerative diseases.
However, advocating for these changes will require data; collecting and analyzing metrics on the impact of neuropathology services on patient outcomes and healthcare costs will be crucial. Demonstrating the cost-effectiveness of timely, accurate diagnoses provided by neuropathologists – particularly in the early detection and management of conditions like Alzheimer’s disease – will provide the evidence needed to support more equitable reimbursement models.
Pathology plays a pivotal role in patient care, but its sustainability depends on fair recognition of the expertise and resources required. By addressing the reimbursement challenges facing our field, we can ensure that neuropathologists continue to provide high-quality, life-saving diagnoses for the patients who need them most.