Glioblastoma is an aggressive cancer that can form in the brain or spinal cord, with an average survival outlook of 12 to 18 months – even with the wide range of treatments available. Where does the disconnect lie between relentless treatment and survival? It’s near impossible to prevent glioblastoma recurrence, meaning that patients face therapy-resistant relapses with a bleak outlook.
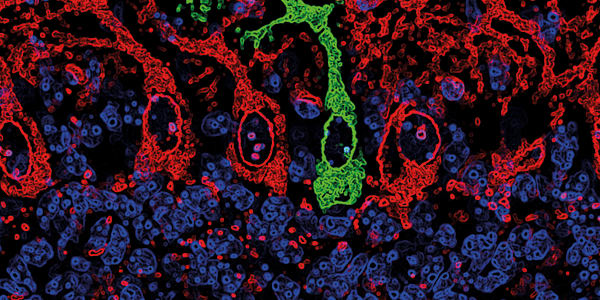
Researchers from the NORLUX Neuro-Oncology Laboratory at the Luxembourg Institute of Health (LIH) decided that we can do better. By reviewing recent literature on glioblastoma plasticity and its role in creating heterogeneous cells, they uncovered several reasons these cancers are so good at coming back (1). Some glioblastoma cells carry stem cell properties, allowing the establishment of heterogeneity that can be difficult to overcome. To make matters worse, glioblastoma cells can also change the way they look and function in response to their environment. This plasticity, combined with the recurring nature of the tumors, makes glioblastoma an even deadlier enemy.

“Cellular states interact dynamically with each other and with the surrounding brain to shape a flexible tumor ecosystem, which enables swift adaptation to external pressure, including treatment,” explained lead author Yahaya Yabo (2). Therefore, the aim of the literature review was to identify insights into potential new treatments that could target the cancer’s plasticity.
The review highlighted the need for a shift in how glioblastoma and other aggressive tumors are treated, but left the door open for exactly which therapies could be effective. “[Glioblastoma] eradication will require targeting the dynamic states rather than single entities,” said Simone Niclou, director of the Department of Cancer Research at LIH (2). “Further studies are needed to reveal the drivers of plasticity and treatment escape. These should address which of the changes are fast and reversible, and which are retained in tumors long after treatment.”

References
- YA Yabo et al., Neuro Oncol, [Online ahead of print] (2021). PMID: 34932099.
- Luxembourg Institute of Health (2022). Available at: https://bit.ly/3Ie3E3r.