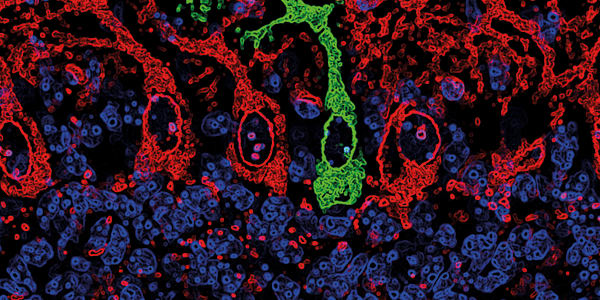
Glioblastoma multiforme (GBM) is the most common primary brain tumor in adults – and the deadliest. Only five to 10 percent of patients survive longer than five years. Predicting prognosis can be particularly difficult because surgical procedures are complicated and invasive, a challenge exacerbated by the tumor’s heterogeneity. But now, a team from the Abramson Cancer Center of the University of Pennsylvania have found that patients with a higher concentration of circulating free DNA (cfDNA) have shorter progression-free survival. Senior author Erica Carpenter believes this underlines the potential utility of liquid biopsy for monitoring brain tumors.
“The assumption in the field is that cfDNA in the peripheral blood is unlikely to be reflective of the tumor microenvironment, which is largely protected by the blood-brain barrier,” she explains. “That’s why we were surprised to find a significant association between pre-therapy plasma cfDNA concentration and clinical outcome.” In a study of 42 patients with newly diagnosed GBM, 28 had a lower cfDNA concentration than the average of the group – and those patients had a median progression-free survival time of 9.5 months. That’s almost double the median 4.9 month progression-free survival time of the 14 patients whose cfDNA concentration was above the group average (1).
The team also discovered genetic mutations in over half of the liquid biopsies – but there was no overlap with the genetic information from solid tissue biopsies. “The mutations detected in plasma, but not tissue, could be an indication of the spatial molecular heterogeneity of the tumor tissue. In other words, the mutational profile of the tumor differs depending on the location of the biopsy tissue,” says Carpenter. This signals a bright future for liquid biopsy in GBM diagnosis. “The combination of liquid biopsy with DNA analysis of the tissue biopsy could improve sensitivity when detecting mutations. A more comprehensive view of the tumor’s molecular profile will enable us to select more effective treatment combinations.” The next step? A larger follow-up study to confirm the findings and hopefully kickstart more personalized treatment for these devastating tumors.

References
- SJ Badley et al., “Clinical utility of plasma cell-free DNA in adult patients with newly diagnosed glioblastoma: a pilot prospective study”, Clin Cancer Res, [Epub ahead of print] (2019). PMID: 31666247.