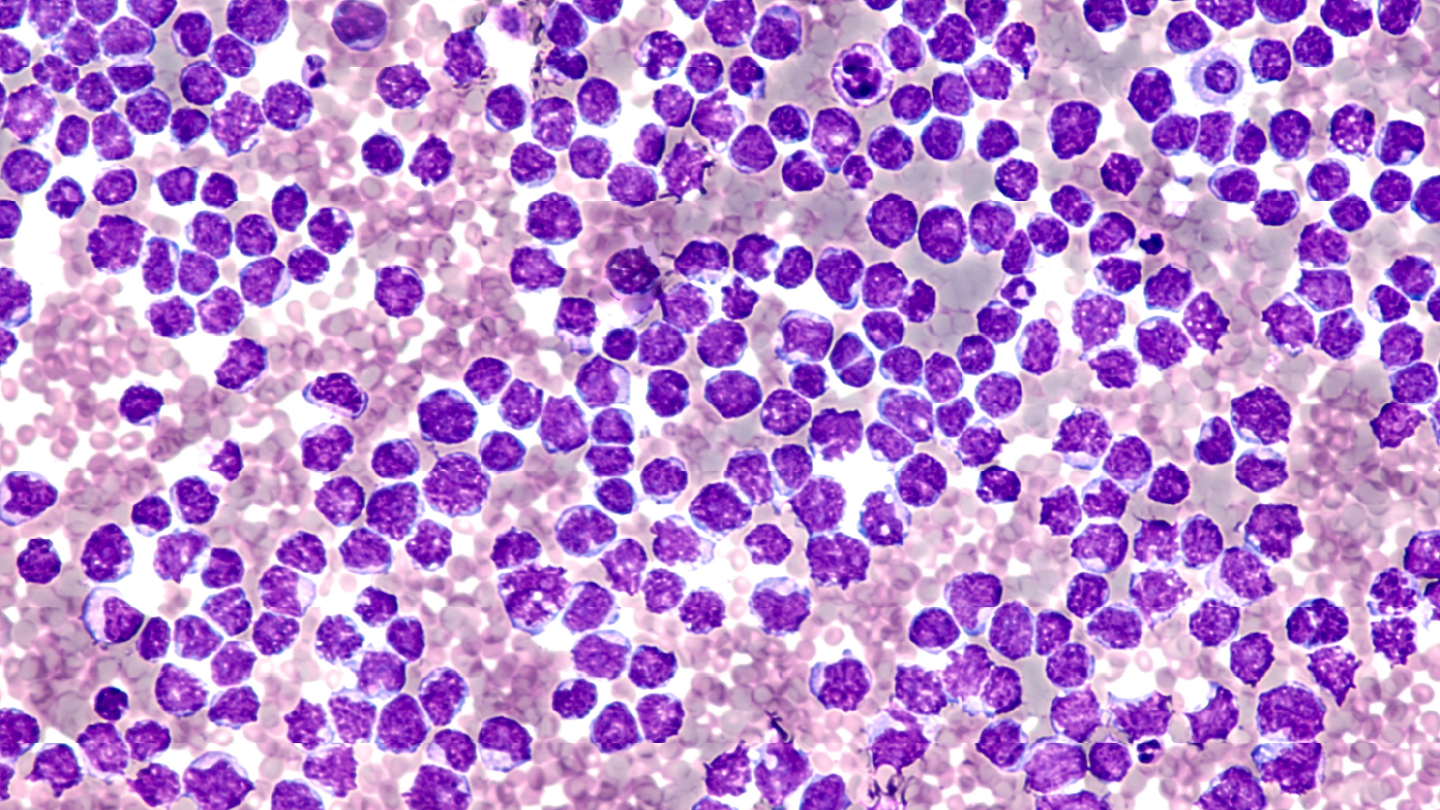
Deletion alterations in two key genes were observed in venetoclax-resistant mantle cell lymphoma cases, suggesting a potential role in resistance mechanisms to targeted therapy, according to a recent study.
Researchers investigated resistance mechanisms and clonal evolution in mantle cell lymphoma (MCL) among patients treated sequentially with Bruton's tyrosine kinase inhibitor (BTKi) and venetoclax. The Hungarian research team employed low-coverage whole genome sequencing (lcWGS) to evaluate copy number alterations (CNAs) across the disease course.
The retrospective study, published in The Journal of Pathology, included 12 patients (median age, 66 years; range, 55–80 years), with 83 percent (10 of 12) diagnosed at Ann Arbor stage IV. Twenty-one formalin-fixed paraffin-embedded tissue samples were analyzed, most frequently from bone marrow (38 percent) and lymph nodes (24 percent). CNAs were widespread, with 91 percent (19 of 21) of samples demonstrating deletions and 71 percent (15 of 21) showing amplifications. Each sample contained at least two arm-level CNAs, with a median of four deletions and one amplification per sample. Post-treatment samples displayed a greater number of CNAs compared with samples collected prior to targeted therapy.
Early progression on BTKi was associated with recurrent alterations in regions encoding NOTCH1, TRAF2, BIRC2, BIRC3, and ATM—genes implicated in noncanonical NF-κB signaling. Alterations affecting these genes were predominantly observed in early progressors, suggesting a potential role in BTKi resistance.
Of the three patients who progressed early on venetoclax, two exhibited deletions in chromosome 9p21.3, encompassing CDKN2A, a gene previously linked to treatment resistance. Patient MCL2 harbored this deletion throughout disease progression and later acquired deletions in SMARCA4 and DLC1, both implicated in tumor suppression and chromatin remodeling. Amplifications in CARD11 and deletions in NOTCH1 and TRAF2 were also found in nonresponders, indicating possible constitutive activation of the NF-κB pathway.
Serial sampling in five patients demonstrated that CNAs evolved during therapy, with new amplifications and deletions emerging at each relapse. The study supports the utility of lcWGS in identifying resistance-associated genomic alterations and highlights deletions in CDKN2A and SMARCA4 as potential biomarkers in double-refractory MCL.




