Dementia doesn’t just affect older people – middle aged individuals can also be affected. But the condition can be hard to recognize. In hopes of improving diagnosis and patient care, researchers at UC San Francisco have taken a closer look at the proteins in cerebrospinal fluid (CSF), identifying clues as to the disease pathogenesis. We spoke with lead researcher, Rowan Saloner, to learn more.

What inspired this study?
Frontotemporal dementia (FTD) is the most common cause of dementia in people under 60, and it can have devastating effects on personality, behavior, language, and movement. Despite its severity, FTD still has no approved treatments and lacks reliable biomarkers for diagnosis or monitoring.
We focused on studying inherited forms of FTD, where we can determine the underlying brain pathology with high confidence even before symptoms begin. One of the biggest diagnostic challenges for FTD is that multiple different brain pathologies can lead to similar symptoms. Unlike Alzheimer’s disease, which now has fluid biomarkers that can identify its pathology in life, FTD still lacks reliable tools to determine what’s actually causing the disease in a given person. We turned to CSF proteomics to tackle this gap.
How might CSF-based proteomic analysis enhance current diagnostic practices, especially when compared to neuroimaging or clinical symptomatology alone?
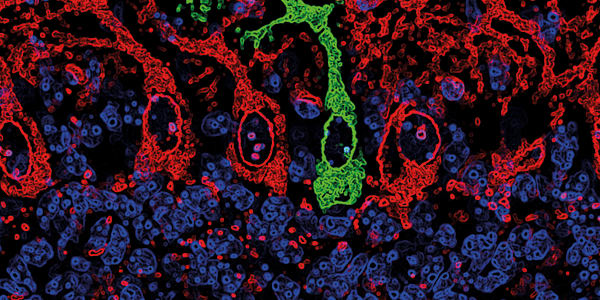
Clinical symptoms and neuroimaging can tell us which neurocircuits are affected in a given FTD patient, but they don’t provide information at the molecular level – whether misfolded tau, TDP-43, or another protein is driving the disease. CSF offers a unique “real-time” window into brain biology because it bathes the brain and spinal cord, making it a rich source of molecular information about neurodegeneration.
CSF proteomics allows us to measure thousands of proteins at once, providing a more precise readout of the biological processes at play, including those that are upstream of neurocircuit dysfunction. This molecular insight could one day help guide personalized treatment strategies, especially as targeted therapies become available.
Can you tell us about your method and your main outcomes – was there anything that surprised you?
By studying spinal fluid from people with genetic forms of FTD, we found specific protein patterns linked to RNA processing, immune activity, and brain cell health. These changes were strongly tied to how severe the disease was, based on symptoms, memory tests, and brain scans. These protein "signatures" give us a real-time view of what’s going wrong in the brain and could help create future biomarkers. Interestingly, we saw similar patterns in people with non-genetic (sporadic) FTD, meaning the findings may apply broadly.
What stood out most was how early some of these protein changes appeared. For instance, proteins tied to RNA and brain cell function were abnormal even in people who had FTD-related gene mutations but no symptoms yet. Some of these proteins could even predict future memory decline. This means molecular changes might start years before symptoms, offering a way to track early disease or develop treatments to delay it.
Were there particular pathways or protein clusters that clearly distinguished frontotemporal lobar degeneration (FTLD) from other neurodegenerative conditions?
Yes – one of the most consistent and surprising findings was a group of proteins involved in RNA splicing, called the spliceosome. These proteins were especially increased in people with mutations linked to TDP-43 pathology (such as C9orf72 and GRN). When we looked at other datasets, we saw that these proteins weren’t as involved in neurodegenerative conditions like Alzheimer’s or Parkinson’s. This is important because TDP-43 normally helps control RNA splicing, and its malfunction in FTD seems to disrupt this system in a way we can detect.
How feasible is it to integrate these CSF protein biomarkers into current diagnostic workflows?
While our study used unbiased CSF proteomics to discover broad patterns of protein changes, translation to diagnostic workflows will likely rely on more parsimonious tools. In practice, single-target assays or small multiplex panels that measure a select set of validated biomarkers will be the most feasible and scalable tools for diagnostic use. A major priority of our work is developing targeted assays based on these unbiased results, particularly for use in sporadic FTD, where genetic screening is not informative.
Could your network analysis approach be used in conjunction with existing diagnostic tools, and how might this improve overall diagnostic confidence in FTLD?
Large-scale protein co-expression network approaches like ours provide a rich, real-time molecular readout of disease biology. While tools like MRI and PET are more easily deployed in clinical settings, they currently lack specificity about the underlying pathological processes in FTD. Proteomic networks can sharpen or validate the relevance of these existing tools by revealing which biological pathways are actively disrupted in a given patient. This integrated approach could improve diagnostic confidence, help refine disease subtyping, and guide more targeted therapeutic development.
What steps are needed to validate and standardize these candidate biomarkers for broader clinical use? Are there plans for multi-center or prospective studies?
To bring these biomarkers into clinical use, we’re developing precise tests on different platforms that can accurately measure protein levels. This will help us set reliable cutoff points and make sure results are consistent across labs and patient groups.
Since FTD is less common than Alzheimer’s, we need collaboration between multiple research centers to validate our findings. We're working with the The ARTFL-LEFFTDS Longitudinal Frontotemporal Lobar Degeneration (ALLFTD) consortium, which includes around 30 sites in North America, and partnering with academic centers that have both fluid samples from living patients and confirmed diagnoses after death.
ALLFTD also contributes to the Global Neurodegeneration Proteomics Consortium (GNPC), which brings together CSF and blood protein data from diseases like Alzheimer’s, FTD, Parkinson’s, and ALS. The goal is to use these combined insights to develop strong, reliable protein-based diagnostic tools.
Do you envision CSF proteomics playing a larger role in differential diagnosis of neurodegenerative disorders in the future?
Absolutely. There’s been a major surge in proteomic research on neurodegenerative diseases, and CSF remains the best way to study the brain in living patients. As we discover more potential biomarkers in CSF, it's crucial to turn those findings into blood-based tests that are easier to use in everyday clinical settings. CSF is the gold standard for finding and confirming biomarkers, especially when trying to tell apart similar brain diseases like FTD, Alzheimer’s, and atypical forms of Parkinson’s.