- Choosing tumor resection margins during neurosurgery can be challenging – but now, a combination of two technologies, Raman spectroscopy and rapid evaporative ionization mass spectrometry, could provide a wealth of tissue data during surgery
- If the technology takes off, it could provide substantial therapeutic benefits, and allow treatment to begin much faster, by removing the long wait for a tissue diagnosis from the lab
- Pathologists are the obvious candidates for getting involved in this new real-time diagnostic approach, because no matter how sophisticated the spectra, tissue experts will be required to interpret and validate the results
- This type of big data is poised to be the future of medicine, and pathologists should embrace the increasing digitization of their specialty in order to remain at the forefront of the diagnostic evolution

As a neurosurgeon, deciding on tumor resection margins can be a daunting task. Removing and analyzing a frozen section is time-consuming, and taking repeated sections during brain surgery isn’t an option. Unlike with other locations in the body where there is a little more room for error, removing healthy tissue in the brain can have serious repercussions – the healthy tissue removed might impact the patient’s balance, speech, ability to concentrate, or worse. But of course, failing to remove all the tumor tissue impacts the patient, too.
Although less than 3 percent of malignancies are located in the brain (1), it affects many children and young adults, and as a result it causes more years of life lost than any other cancer. And because it’s so rare, funding new technologies and studies can be difficult. Both Kevin O‘Neill, consultant Neurosurgeon at Imperial College Healthcare NHS Trust, and I found the lack of options for treating our patients frustrating, and the particular challenges brain cancer poses during surgery set us out on a quest to tackle them head on. During our investigations, my colleagues and I opted to study two separate but very complementary technologies: Raman spectroscopy, and rapid evaporative ionization mass spectrometry (REIMS). Together, we believed they could bring the diagnostic abilities of the lab right into the operating theatre.
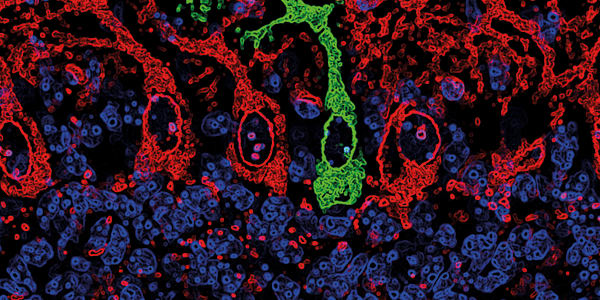
Raman spectroscopy is optical, involves no destruction of tissue, and gives the surgeon advanced warning that tissue may be abnormal, allowing them to make a decision on whether or not to remove it. A recent study has shown the technology to have 93 percent sensitivity and 91 percent specificity in distinguishing normal tissue from tumor in the brain (2). As tissue is being cut, REIMS provides constant positive feedback that the tissue being removed is indeed cancerous. When the surgeon hits normal tissue, the system will alert them. In a previous intraoperative study involving patients with various cancers (including brain cancers), REIMS analysis of brain tissue matched the histological findings 100 percent of the time (3). Although both of these technologies are valuable in themselves, the way they interact amplifies their value (see “In Harmony”). This combined approach teams a quick and accurate way to predict what’s ahead, with a reliable, detailed analysis of the tissue currently being operated on – a fantastic combination!
Raman spectroscopy:
- Raman spectroscopy, which is commonly used in chemistry, relies on scattering of light from a laser, which interacts with the molecules of the tissue it’s aimed at, providing vibrational information
- This information offers spectral tissue characteristics based on the molecules present
- This system can be used in real-time to distinguish between the molecular signature of normal and cancerous tissue
- REIMS uses bipolar forceps, which are routinely used during surgery, to cut tissue and control bleeding, to analyze the smoke produced as tissue is cut
- The gas-phase ionic species produced during cutting are sucked up for analysis by mass spectrometry
- The mass spec profiles are specific to the tissue and statistical analysis can provide information on the tumor, including grade in some cases
We have now tested the two technologies in over 20 patients during surgery, and the method has demonstrated the ability to spot and grade tumor tissue. It’s not yet been validated, so it can’t be used for a definitive diagnosis, but it appears to characterize tumors very well based on initial results. The technique we’re using has also garnered a good deal of media attention – in fact, the surgery of one of our patients was filmed by the BBC (4), and covered by numerous media channels. During surgery, the patient was asked to speak and sing in order to ensure these abilities weren’t affected by the section of brain we were removing. We demonstrated the precision of this combined technological approach, and it was pretty impactful to watch, hence the media attention that came with its filming.
I see these two technologies as having three areas of clinical potential. First, they could provide an immediate diagnosis, avoiding the often nerve-wracking waits of a week or more for histological results. For a patient who may have felt perfectly healthy, and has been told they could have brain cancer, this wait is extremely difficult. Further, attaining an accurate diagnosis on the day of surgery means that treatment can be streamlined, allowing for a personalized treatment plan to be devised in a fast and efficient manner, much earlier than is otherwise possible. Second, it can provide a continuous data flow to the surgeon and therefore a whole new layer of information to aid decision-making in the theatre. Current methods, such as preoperative MRI and ultrasound, leave a lot to be desired, and I know that many neurosurgeons would really value these extra sources of information to work with. Finally, there are clear implications for personalized medicine. Each time REIMS is used, it generates around 2 million spectral points – that’s a lot of data. The extreme level of analysis we achieve with REIMS could help to create the ultimate patient profile, and identify diagnostic biomarkers – it should be possible to mine the data and find out if particular spectrums perhaps predict response to treatment, or disease aggressiveness.
On hearing of a technology that could potentially diagnose tumor tissue in real-time during surgery, some surgical pathologists may think: “But you’ll put us out of a job!” Actually, nothing could be further from the truth. Pathologists are poised to play a crucial role in these new developments – as long as they embrace the way diagnostics are evolving. These spectra provide additional tissue information which could aid their own diagnostic work; sampling errors during biopsy can result in inaccurate diagnoses. This technology also offers a faster route to diagnosis – with many tools at pathologist’s disposal, such as immune-staining and genomic analysis, getting an answer takes time. With REIMS, the answer is instantaneous. I believe that pathologists are perfectly placed to become the specialists in this technology, advising surgeons on the spectral information being collected in the theatre. After all, as the surgeon acquires this new tissue information, they will need a tissue specialist to guide them. In future studies, it would be great to get more pathologists involved so they can define their own role.
Society is becoming more and more data-rich, and the more available data, the easier it is to classify and characterize disease. Although I believe technologies like this are the future, a human will always be needed to assess if the system is reliable or not. We cannot replace histologists! But we don’t just need the input of pathologists – I find these new technologies so exciting because they are truly cross-disciplinary. It will need pathology, chemistry, physics, electrical engineers, surgeons, and nurses – motivated scientists from many disciplines – to get involved.
So is it likely that the Raman probe and REIMS will gain widespread adoption in the real-time diagnostic setting? As with any new innovation, it is too soon to predict its eventual success or failure. But so far, with the feedback I’ve had from conferences and colleagues, I am very hopeful. As is always the case though, obstacles exist. Using these devices in surgery is simple, as it’s essentially a “point and shoot” approach. Interpreting the spectra is a more complex matter, but we are currently developing algorithms to better understand the data the analysis generates, and hope to implement a simple system to distinguish between normal and tumor tissue. Expense is another problem. At the moment, these are expensive pieces of kit used for research; especially REIMS. But they’re equipped with more dimensions than are needed – we won’t need everything to be analyzed. Once it’s clear what information is important to us, it should be possible to slim down the system. Much like modern smartphones, I expect these tools will become smaller, lighter, and better; and older versions will become progressively cheaper. One key factor that would support a cost-efficiency argument is that these technologies can be used in other cancer types – the Raman probe has already been trialed in upper gastrointestinal tract malignancy, and colon cancer. REIMS is also being investigated in breast, colon and gynecological cancers. I think in the next five years, we are going to see expansions of these technologies and the different situations they can be used in, as they represent a potential game-changer for many types of surgery. Now that proof-of-concept has been established, larger, interventional studies need to come next.
Cost and training aren’t the only issues: for this technology (and others like it) to succeed, I think it’s important that pathologists embrace the increasing digitization of their discipline. Essentially, this technique is transforming tissue into digital information, which we can then use to profile the patient. Looking further into the future, I definitely see techniques like this becoming widespread. It gives the surgeon a quick answer, and learning how to further use this kind of complex data is simply a part of modern medicine. With any large change there is resistance; many people tend to be happy with the status quo, but I suspect that, as the applications of this type of technology are more widely understood, it will eventually win over the skeptics.
Babar Vaqas is a neurosurgeon at the Imperial College Healthcare NHS trust, London, UK, and chief investigator of the Raman spectroscopy and REIMS trial. The project is supported by the BTRC (Brain Tumor Research Campaign) and BTR (Brain Tumor Research).
References
- Cancer Research UK, “Brain, other CNS and intracranial tumours incidence statistics”, (2014). Available at: http://bit.ly/1L6b6si. Accessed October 7, 2015. M Jermyn, et al., “Intraoperative brain cancer detection with Raman spectroscopy in humans”, Sci Tranl Med, 7, 274ra19 (2015). PMID: 25673764. J Balog, et al., “Intraoperative tissue identification using rapid evaporative ionization mass spectrometry”, Sci Transl Med, 5, 194ra93 (2013). PMID: 23863833. BBC News, “Laser detects brain tumour cells during surgery”, (2015). Available at: http://bbc.in/1K2Bc45. Accessed September 28, 2015.