Diagnosing neurodegenerative diseases like Alzheimer’s can be a hit and miss process – but is a lab-based test on the horizon? By Roisin McGuigan
- Current tests for neurodegenerative disease aren’t perfect, and can lead to misdiagnosis – it is estimated that up to 20 percent of Alzheimer’s diagnoses could be incorrect
- The race is on to develop an alternative to clinical assessment – including lood-, breath-, skin- and spinal fluid-based tests
- Here, we hone in on four research teams hoping to be one of the first to develop an accessible and sensitive diagnostic technique
- Any that succeed would have a huge impact on both clinical trial recruitment and patient management, but there is still some way to go before this becomes a reality
Diagnosing age-related neurodegenerative disorders (NDs) is a challenge. In the clinic, the diagnosis of Alzheimer’s disease (AD), Parkinson’s disease (PD) and other age-related dementias relies on a mixture of clinical assessment of cognitive symptoms, brain imaging, and the measurement of proxy biomarkers. But these methods are far from ideal – the only way to obtain a definitive diagnosis of AD, for example, is by pathological examination of brain tissue after death – and it goes without saying that this has little direct application to patient diagnosis and management.
The overlap of symptoms between the various forms of ND can also result in misdiagnosis – especially during the early stages of disease, or in younger sufferers, leading to inappropriate treatment and unnecessary medication (1). With an aging population and a growing number of affected patients, a more objective, lab-based method for diagnosis is becoming a more urgent research goal; so it’s no surprise that research groups around the world are working on innovative new approaches for diagnosing – and differentiating – NDs. We take a look at four potential approaches, and speak to some of the researchers working to solve this pressing problem.
A research team from the Israel Institute of Technology appear to have found a way to identify patients with PD using only their breath – by measuring exhaled organic compounds, they were able to distinguish between patients with idiopathic PD, those with non-idiopathic PD, and healthy controls. “The patient breathes through a device which collects the compounds in their breath,” explains co-author of the associated paper (2), Hossam Haick, “these are then exposed to a nanoarray composed of sensors, combined with pattern recognition algorithms, which can be trained to recognize disease-specific breath signatures,” (Figure 1).

Haick believes the test represents an improvement over current methods; “Physician evaluation is linked to high misdiagnosis rates, and expensive and risky imaging techniques will only be helpful in a limited number of specific cases. Our approach is noninvasive, inexpensive, fast and doesn’t require an expert to operate, making it suitable for large scale screening of high risk populations.” Haik and lead author of the study, Morad Nakhleh, say they hope their test could be used clinically in the future – but with an accuracy of 84 percent, they plan to increase the sensitivity first. “The test will not replace pathological examination” adds Haick, “as it provides the only direct proof of disease. But we plan to validate our breath test technology and determine its potential in stratifying patients into disease subtypes.” Eventually, the group hope to study people with genetic susceptibility to PD, with the aim of early detection, before clinical symptoms appear. “This would allow us to administer preventative treatments such as neuroprotective agents, once such therapies become available,” says Haick.
Meanwhile, researchers from San Luis Potosi, Mexico believe that skin could contain revealing clues about neurocognitive health, including conditions such as AD and PD. “Until now, pathological confirmation was not possible without a brain biopsy, so these diseases often go unrecognized,” says study author Ildefonso Rodriguez-Leyva. The researchers hypothesized that since skin and brain tissue have the same embryonic origins, they might also display the same abnormal proteins found in some NDs. In a small study population of 20 patients with AD, 16 patients with PD, 17 patients with dementia caused by other conditions, and 12 healthy controls, they obtained and tested very small skin samples from behind the ear, to see if they could identify altered proteins indicating AD or PD (3). They observed that in patients with PD or AD, levels of tau protein were seven times higher when compared with healthy patients and those with dementia from other, non-degenerative causes. Patients with PD also had eight times higher levels of α-synuclein protein than the healthy controls – a promising find not only for diagnosing dementia, but for identifying the underlying disease. “More research is needed to confirm these results,” admits Rodriguez-Leyva, “but the findings are exciting because we could potentially begin to use skin biopsies from living patients to study and learn more about these diseases. If our findings are shown to be consistent, we could have an innovative, accessible way to support clinical diagnosis using skin biopsy. Because even in the best neurological centers, diagnosis can be erratic, and only defined by the progression of disease symptoms, or using expensive biomarkers that aren’t always accessible.” In the future, Rodriguez-Leyva and his team hope to culture live tissue to enable better understanding of the mechanisms involved in the disease, and to work on the development of an autologous vaccine against protein deposits.
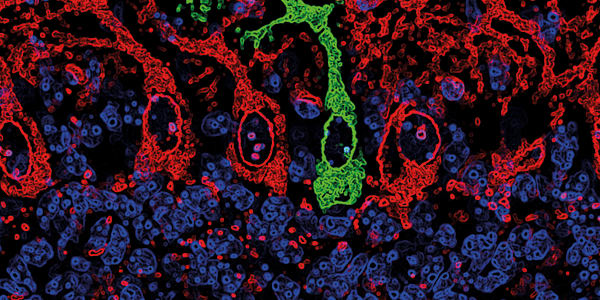
An approach that could be deemed controversial by some, owing to its invasive nature, is nonetheless showing some promise and that is in the testing of cerebrospinal fluid for the biochemical diagnosis of AD (4). The method is based on the premise that misfolded amyloid-β (Aβ) peptide oligomers accumulating in the brain, causing cellular dysfunction and damage to tissue, play an important role in the pathogenesis of AD. These oligomers have been found to circulate in biological fluids, but only in very small quantities that were difficult to detect – until now. Researchers from the University of Texas, USA, and the University of Milan, Italy, have developed a sensitive assay for detecting very small amounts of Aβ oligomers, by creating a method for cyclic amplification of the misfolding process in vitro. They then tested the cerebrospinal fluid of 50 patients with AD, 39 controls and 37 patients with non-AD NDs, and achieved an impressive 100 percent sensitivity when distinguishing patients with AD from patients with non-AD ND, and high levels of sensitivity and specificity for distinguishing the different sets of patients (Figure 2).

However, even if spinal fluid testing has a high level of accuracy, lumbar puncture is a highly invasive and inconvenient test, which carries a risk of nerve damage – but the authors hypothesize that Aβ oligomers may be circulating in other fluids, and in the future, they may be able to detect the biomarker using a more routine blood test.
Finally, there’s a team that believes they could have found a way to introduce a simple blood test into AD testing. The creation of compounds that can bind to amyloid in the brain and then be detected via PET scan has been credited as a key breakthrough for AD research, and trials of anti-amyloid agents that could potentially halt disease progression are now underway. But screening for potential clinical trial participants using PET will unavoidably expose patients who are amyloid-negative and cognitively normal, to harmful radiation, especially in larger study populations. Could there be a safer alternative? A research team from the University of California, Los Angeles (UCLA), USA, in collaboration with the International Alzheimer’s Disease Neuroimaging Initiative, may have found a solution – a multimodal approach for predicting brain amyloidosis using cognitive assessment, brain imaging, and a simple blood test.
“For AD, the gold standard is always a pathology diagnosis – what is going on in the tissue, what abnormalities are we finding under the microscope? But it’s not easy to access the brain and take biopsies in a living subject,” says lead researcher Liana Apostolova. “So we need to look for other metrics to help us make a diagnosis. There is no perfect biomarker for Alzheimer’s, so over the last five years or so, increasing attention has been devoted to studying several biomarkers at a time, rather than just a single one,” she adds. Apostolova and her team combined a series of measurements, including memory tests and structural MRI (information that is routinely obtained during clinical work-up for suspect AD cases), along with several blood proteins known to be associated with AD, and achieved a test sensitivity of 68 percent, and a specificity of 78 percent (5).
“People think AD is confined to the brain, but it leaves a signature in the periphery,” says Apostolova, “many blood proteins change during the disease process – this means in even the most rural settings, with no PET scan available, you can get a blood draw and predict brain amyloidosis and therefore AD.” If there is wide uptake of the test, it won’t only have implications for diagnosis and management of AD, adds Apostolova. “Since amyloid PET imaging has been developed, we’ve found that around 20 percent of patients clinically diagnosed with AD do not have amyloid deposits in their brains. So not only have they been misdiagnosed and unnecessarily treated, they may also have been entered into clinical trials when they are not suitable candidates. And increasingly, we are looking at the early and presymptomatic stages of the disease, and in these cohorts amyloid-negative individuals may make up as much as 50 percent of your study population – that’s a 50/50 chance that they aren’t suitable!” she emphasizes. The creators of the test envision it as playing an important role in clinical trial design – potential participants could be pre-screened using the blood test to predict which individuals are amyloid-positive, which could significantly decrease the risk of exposing amyloid-negative patients to PET radiation. The next step? “We are continuing to look for even more powerful predictors in the blood,” confirms Apostolova.
It is clear that a reliable, noninvasive lab test for diagnosing complex neurodegenerative diseases could be a boon for both clinicians and researchers, allowing for better diagnosis and management for patients, and in future, identifying patients in the presymptomatic and early stages of disease. It could also help researchers target appropriate candidates for their studies, and identify which patients may benefit from inclusion in clinical trials – which could, in turn, have a great impact on the development and validation of effective therapies. But with so many innovative approaches currently in the works, it remains to be seen which will make it into clinical practice.
References
- JE Gaugler, et al., “Characteristics of patients misdiagnosed with Alzheimer’s disease and their medication use: an analysis of the NACC-UDS database”, BMC Geriatr, 13, [Epub] (2013). PMID: 24354549. MK Nakleh, et al., “Distinguishing idiopathic Parkinson’s disease from other parkinsonian syndromes by breath test”, Parkinsonism Relat Disord, 21, 150–153 (2015). PMID: 25511331. American Association of Neurology, “Skin test may shed new light on Alzheimer’s and Parkinson’s diseases”, (2015). Available at: http://bit.ly/1NWo8K7. Accessed on April 9, 2015. N Salvadores, et al., “Detection of misfolded Aβ oligomers for sensitive biochemical diagnosis of Alzheimer’s Disease”, Cell Rep, 10, 261–268, (2014). PMID: 24656814. LG Apostolova, et al., “Brain amyloidosis ascertainment from cognitive, imaging and peripheral blood protein measures”, Neurology, 84, 729–737 (2015). PMID: 25609767.