I first began studying the impact of enriched environments on aging changes in the brain during my PhD studies at UC Berkeley and it was as a postdoc at Boston University that I became particularly interested in iron in the brain.
Thanks to our early work, it is now generally accepted that iron plays a key role in the development of Alzheimer’s. There are still, however, several key knowledge gaps that need to be filled.

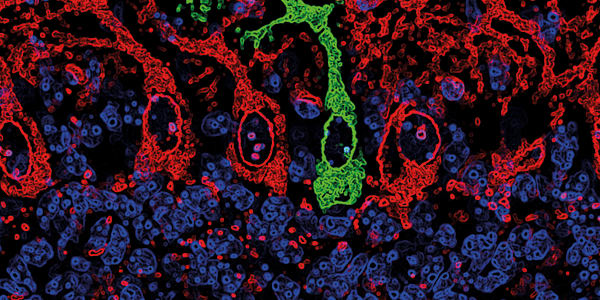
So let’s look at what we know. We have shown that iron dyshomeostasis occurs in the brains of Alzheimer’s patients and this excess iron promotes plaque and neurofibrillary tangle formation. Crucially, our work has allowed us to identify a mutation in the HFE gene that we now know to be present in around 30 percent of Caucasians with Alzheimer’s. We began looking at the HFE gene and its mutations because of its association with the iron overload condition known as hemochromatosis. When we first started no one thought the HFE mutation would change brain iron status, but we and others have shown that it does. We also know that the mutation, in the presence of the APOE4 allele, increases a person’s likelihood of developing the disease. We have also identified that the HFE gene variant impacts white matter status, which has been shown to affect cognitive performance. These are groundbreaking discoveries. But we are faced with many questions: what genetic-environmental interaction predisposes a person to Alzheimer’s? How can we restore iron homeostasis given the critical importance of iron in so many enzymatic reactions? How likely will someone with the HFE mutation go on to develop Alzheimer’s? What processes are specifically disrupted that lead to iron dyshomeostasis? The field is so complex. What we need is to build a profile of the disease and all of the different influences that determine its development, and this is what I am focused on. To demonstrate the challenges that we are faced with, let’s hypothetically suggest that dietary iron intake is reduced, or iron chelators administered, in at risk populations. Studies have shown a correlation between anemia and cognitive decline in the elderly. So, although giving iron chelators is showing some promise in clinical trials in the UK and France in Parkinson’s disease, this may not be right for Alzheimer’s patients. If we look at cholesterol; there are three steps in the formation of cholesterol in the brain that are absolutely dependent on iron, which means that its synthesis is going to be disrupted if there is iron dyshomeostasis in the brain – and there are good examples in the literature of the association between decreased brain cholesterol and Alzheimer’s. As a result, we are now questioning if cholesterol-lowering statins should be used in those people who are at risk of neurodegenerative disease, and data are beginning to emerge that urge caution in their use in Parkinson’s disease, multiple sclerosis and in ALS. Researchers haven’t looked at this issue in Alzheimer’s yet, but I think the iron and cholesterol story needs to be visited pretty quickly and aggressively in a population-based study. We are very excited by the outcomes of some of our recent work, which we will be publishing soon, where we have shown a disruption in brain cholesterol in an animal model of the HFE mutation with similar findings in humans that have the same mutation. If we consider what we know about HFE; although we have shown that a mutation in this gene is present in 30 percent of people with Alzheimer’s, around 10–15 percent of the general population also carry it, the majority of whom are unaffected by hemochromatosis, and this is puzzling. So we’re working to understand if there is a gene-environment interaction that, somewhere along the iron pathway, puts a person in a position that they will develop iron dyshomeostasis and Alzheimer’s at some point later in life. We know that this is not a condition that is caused solely by a genetic mutation. So the $60k dollar question: what precise changes cause the brain to lose iron homeostasis as it ages? Is it genetic? Are there signals in the brain that become altered and make the brain think it needs more iron than it does? We just don’t have a good answer yet. We need to better understand the processes that lead to tangle and plaque formation, and iron’s role, and my hope is that these processes will become our therapeutic target. Even though iron is involved in forming those pathogenic processes, we may want to leave the actual iron alone. Chelating iron is probably not the answer, and probably neither is limiting iron in the diet. The race is on to find an effective therapeutic target. Is it an iron chelator, an anti-amyloid vaccine, an anti-oxidant, an anti-inflammatory? Is it a combination of more than one? This is what we don’t know. But what we do know from testing in clinical trials is that sometimes things work in some patients but not all. I believe at some point along the biological pathway to dementia, it becomes a common pathway, and the challenge for us as scientists is to find that common point. If we’re lucky enough to do that, we’ll have found our therapeutic target. Our biggest opportunity to make an impact in Alzheimer’s right now is to catch it early and to limit any cognitive decline before it becomes problematic. The way we’ll do that is to combine genotyping, biomarkers and imaging, with iron and cognitive testing. A blood test alone won’t cut it; there is a lack of agreement on the serum levels of iron and iron proteins and the impact of those levels in the brain. The same is true of copper and probably cholesterol. What’s in the blood doesn’t always inform us very well of what is going on in the brain, so we’ll need all of those additional pieces of information. My ideal vision would be for people from the age of 50 to get full genetic, image and cognitive profiling and for us to use the knowledge we gather from those assessments to highlight a person’s risk of later Alzheimer’s development. We can then provide the adequate guidance to delay and even perhaps prevent progression to full blown dementia. Right now, we’re not able to do that. We need to define a risk profile first. It’s the missing piece of the puzzle that’s needed for early diagnosis and, importantly, prevention. I think we’ll get there in the next 20 years though. Looking back on my career, I feel proud that our research has defined a clear relationship between iron and Alzheimer’s; when we first started out, nobody was looking at iron in the brain and its connection to neurodegenerative disease. What would really make me feel good at the end of all of this would be to know that we’ve really made a significant contribution to elucidating those biological processes that lead to dementia. I’m hoping that all of our work on genetic profiling, the influence of iron on tangle and plaque formation, will help us get to that therapeutic target. I wish I could say to someone that if you have the HFE mutation then you are going to get Alzheimer’s and we can fix that, but that is totally unrealistic. I am absolutely focused on researching this gene-environment interaction. I want to find if there is some form of intervention strategy around iron that makes people better. If we do that, I will feel like our research has made a contribution and I will be happy.

James Connor is Distinguished Professor of Neurosurgery, Neural and Behavioral Sciences and Pediatrics, Vice Chair of Neurosurgery Research and Director of the Center for Aging and Neurodegenerative Diseases at Penn State University, MS Hershey Medical Center, USA.

- JR Connor et al., “A histochemical study of iron, transferrin and ferritin in Alzheimer’s diseased brains”, J Neurosci Res, 31, 75–83 (1992). PMID: 1613823.
- JR Connor et al., “Is hemochromatosis a risk factor for Alzheimer disease?” J Alz Dis, 3, 471–477 (2001).
- MD Meadowcroft et al:, “MRI and histological analysis of beta-amyloid plaques in both human Alzheimer's disease and APP/PS1 transgenic mice”, J Magn Reson Imaging, 29, 997–1007 (2009). PMID: 19388095.
- G Bartzokis et al., “Prevalent iron metabolism gene variants associated with increased brain ferritin iron in healthy older men”, J Alz Dis, 20, 333–341 (2010). PMID: 2016457.
- F Ali-Rahmani et al., “HFE gene variants, iron, and lipids: a novel connection in Alzheimer’s disease”, Front Pharmacol, 8, 165 (2014). PMID: 25071582.
- M Meadowcroft et al., “The effect of iron in MRI and transverse relation of amyloid-beta plaques in Alzheimer’s disease” NMR Biomed, 28, 297–305 (2015). PMID: 25530083.
Untangling Tau by Brad Hyman
The Overactive Brain by Michela Gallagher
Food for Thought by Ewan McNay