Telepathology for Everybody: Part 2
Meet the pathologists bringing telepathology to low-resource settings
Helen Bristow | | 10 min read | Interview

Joe Knapper, Kelsey Hummel, Daniel Rosen, and Elisée Hategekimana at CHUB
Credit: Joe Knapper
There are some hospitals in the world whose patients are asked to take their own histology samples to the nearest facility with the requisite testing capacity. Many pathology labs are battling with intermittent power, water supply, and internet connections. Thankfully, there are pathologists who are determined to empower labs to provide the very best health care despite these obstacles.
Pathologists Daniel Rosen, from Baylor College of Medicine, and Kelsey Hummel, from MD Anderson Cancer Center, are two such problem solvers. They teamed up with the inventors of the OpenFlexure digital microscope – an open source device that can be 3D printed, constructed, and maintained on site – to bring telepathology to hospitals with even the most limited of resources.
The team started 2024 with a trip to Rwanda to field test the device. In collaboration with pathologist Elisée Hategekimana at the University Teaching Hospital of Butare (CHUB), they printed, constructed, and tested OpenFlexure microscopes, then trained the pathology team how to use them. We sat down with Rosen and Hummel to find out more.
See part one of this article to learn about the design and development of the OpenFlexure digital microscope.
Please tell us what you do and how you became involved with world health projects…
Kelsey Hummel: I am currently doing a subspecialized fellowship in cytopathology at MD Anderson Cancer Center and I will be going to the University of Michigan to pursue another subspecialty fellowship in gynecologic pathology. My interest in global health started back in 2018, when I took my first trip to Peru to bring parasitology testing to communities along the Amazon river near Iquitos. I saw there was a real need for someone in pathology to provide input on how to provide laboratory diagnostics in low-resource settings, with a focus on providing the best patient care for that population.
Daniel Rosen: I’m a professor of pathology at Baylor College of Medicine and I work at the Veterans Affairs Medical Center in Houston, Texas. I’m also a board certified pathologist in both anatomic and clinical pathology. I recognized the need for an affordable and sustainable telepathology device during my trips to China, Brazil, and Honduras back in 2017–2018. I was conducting a research project requiring the review of thousands of biopsies for screening of stomach and esophageal carcinoma, and I noticed that there was a huge delay – sometimes up to a month – on the processing of these biopsies. That meant that some had to be reviewed after my return to the US. I requested images of the slides, but they were very poor quality, taken with camera phones. That got me thinking how great it would be to have a low cost, low resource, energy efficient telepathology device to capture images on site.
How did you become involved with the OpenFlexure project?
DR: I created a prototype telepathology device with my team by attaching a camera from a cell phone to the objective lens from a microscope and creating a moving platform for the slide. We got a few nice pictures – but it was really hard to operate.
I started doing some research into a flexure mechanism that could be 3D printed and that led me to the website for the OpenFlexure microscope. I immediately contacted the inventor, UK-based Richard Bowman, and we started working together. He sent me some 3D model files, I bought a 3D printer, set it up in my garage, and embarked on a very steep learning curve. After about six months, I had a working prototype of the microscope and software, repurposed as a clinical device. And then I took it to Brazil and we did our first validation study, looking at esophageal biopsies for dysplasia.
KH: In 2019, I started my residency at Baylor College of Medicine, which is where I met Daniel Rosen and learned about his world health initiatives in China and Brazil. When I was awarded the American Society of Clinical Pathology fellowship grant in 2021, I made my first connection to Hategekimana in Rwanda, and I talked to Daniel about how we could help improve the pathology department at CHUB. He immediately recognized the potential of the OpenFlexure device in that setting.
What did you learn from the validation study?
DR: Our paper has now been published – and it was a really surprising result. We achieved a high concordance among pathologists who used the OpenFlexure digital microscope for dysplasia diagnosis. Because of these results, we started looking at other possibilities in health care. I was working with Kelsey on a global health project in Rwanda that I thought might benefit from the OpenFlexure capability. We then started working almost full-time on the microscope with Richard Bowman and Joe Knapper at the University of Glasgow.
How difficult was it to secure funding for the Rwanda project?
KH: The first hurdle was finding an accessible source. Big grants, from the NIH, for example, depend on a percentage of your time or salary being dedicated to the research. Those are very difficult for Fellows to secure. We quickly learned to apply for smaller grants, such as the College of American Pathologists’ Global Development Grant, that had a better chance of being awarded to trainees.
The other consideration was finding a way to get funds to Rwanda. That was really important to us, because one of the aims of the project was to test the feasibility of building OpenFlexure devices on site in the country, using locally sourced components, rather than ordering them in the States and shipping them over. In addition, bringing supplies into the country via luggage has its own challenges with customs and tax considerations. For example, when a piece of lab equipment is donated, the receiving country may have a 20 percent tariff on these items. Some of these devices are tens to hundreds of thousands of dollars, so you can imagine what the tariff would be. Unless you pay it, the machine just stays at the airport. We were very fortunate to partner with a non-governmental organization in Rwanda, Innovation for Perfection in Health (IPH), which received the funds from the grant. It’s led by pathologists and medical technologists, and its goal is to help increase access to medical services in the southern province of Rwanda.
The final consideration was that the funding didn’t cover travel and accommodation costs. You have to find a way to self-fund those things, which can be really difficult, especially for trainees.
How did the testing go when you got to Rwanda?
DR: At first, we thought everything was against us: the flight was cancelled the day before departure, the car broke down on the way to Butare, the installation process took longer than expected… Once we arrived, we were faced with power outages, poor internet connections, problems with the sample preparation processes… We really did not anticipate the extent of the lack of resources in Rwanda. But we fixed all the problems, one by one, and had a great experience working with Hategekimana’s team.
How did the pathologists at CHUB respond to the kit?
DR: It was a fantastic reception. The team at CHUB saw a world of possibilities opening up for telepathology, teleconsultations, and educational sessions. We had a 15-minute meeting scheduled with the hospital leadership that ended up as a two-hour talk about the microscope and all the other possibilities that could open with the installation of these microscopes.
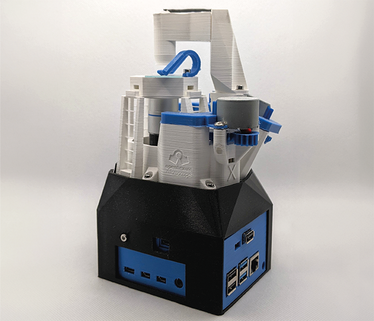
An assembled OpenFlexure microscope
Credit: openflexure.org (CC-BY)
What’s your vision for the role of the OpenFlexure device in healthcare settings?
KH: I can see a clear benefit in pathology education. Without access to multiple or multiheaded microscopes, it can be difficult to train groups of students together. The OpenFlexure microscope allows the slide to be scanned and then displayed and manipulated on a standard monitor or screen, allowing a better teaching/learning experience.
DR: Pathologists can do a lot with telepathology in terms of training, monitoring, and diagnosis. I think that a low cost, low maintenance, and power efficient device like the OpenFlexure microscope can open all these possibilities for pathologists. We need to run a lot of validations, but the option is this or nothing.
I can give you an example of what can go wrong with lab equipment: in Butare, there was an autoprocessing machine that no-one could use because the rubber belt was broken. It would be so easy to fix, but they could not find the part in Rwanda. The OpenFlexure microscope, on the other hand, is designed to be maintained in house – there’s no service contract required. All the parts should be readily available, so we just need to teach the pathologists and technicians how to build, operate, maintain, and fix the device themselves. We don’t want to just go into hospitals, run a project, write a paper, and leave. To use an analogy, we want to teach them how to fish and give them a fishing rod.
What else have you learned about pathology in hospitals with limited resources?
KH: The pathologists at CHUB were frustrated by having to send away some of their specimens to other hospitals for additional testing. The patients were frustrated by sometimes needing to travel to another city to receive the care that they needed. Hategekimana and his team would like to be able to run a service that’s comparable with their other referral hospitals, but there are significant obstacles to that. They need to make sure they have enough revenue to be able to cover the additional testing that they want to do. There are also analytical factors, such as making sure the tissue is processed correctly to be able to do this additional testing or being able to get the specimens grossed and evaluated in a timely manner. But if they only receive three specimens a day, for example, there is little point in trying to run the processor every day when it would be more efficient for them to process all the cases together once a week.
My point is that, when you’re trying to work with limited resources, you need to understand the reasons for the current processes. Only then can you start thinking about ways to improve systems and make them sustainable. It’s important not to try to fix problems, but to help your peers find long-term solutions.
What do you have planned next?
KH: The first thing we need to do is to find more funding. It’s actually more difficult than you would think to find small grants. That said, we are trying to find cost-effective solutions to problems, so we don’t need to ask for millions of dollars. The funders for the Rwanda project were really impressed that our application was for less than $5,000. We only applied for what we needed, and that in itself opened up funds for other applicants. But those small pots are surprisingly hard to come by.
We’re specifically looking for grants that are focused on cancer diagnosis, cancer care, or infectious disease. The Director of CHUB was very interested in malaria testing capabilities, for which our OpenFlexure collaborator, Joe Knapper, has a lot of experience. I have a meeting soon to discuss some grant ideas with Hategekimana. He will be able to give us a better idea as to whether these ideas are feasible or if we need to change course to do something different.
Combining my dual backgrounds in science and communications to bring you compelling content in your speciality.