The Devil is in the Detail
How to optimize the preclinical pathology applied to cellular therapeutics
At a Glance
- Recent developments have rendered the rapidly developing field of cell-based therapies more palatable to the public
- The regulatory requirements for preclinical safety and efficacy studies for cellular therapeutic agents tend to be much more fluid than for conventional drugs and small molecules
- Pathologists need to be able to demonstrate the presence of the cells in the tissues of the host animal, show the continued viability of those cells, and confirm that the cells are differentiating into the intended cell type
- Careful selection of biomarkers and animal models, together with tissue triage and DNA technologies can help you design a high-quality study at lower cost
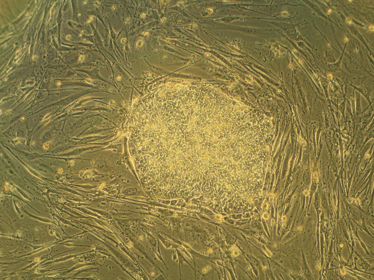
By Ryddragyn at en.wikipedia via Wikimedia Commons from Wikimedia Commons
The development of stem cell-derived cellular therapeutics has long been dogged by controversy. Cell-based medicines have been hailed by some as the panacea of all ills, while others have seemingly declared them the root of all evil. These therapeutic agents fall under the umbrella of regenerative medicine because they are intended to restore or replace the structure and function of damaged organs, thereby curing previously untreatable injury or disease. In recent years methods have been developed that allow the harvest of stem cells from embryos without causing embryonic death, and for the induction of pluripotency in adult cell lines. These developments have rendered such therapies more “palatable” to the public, and today, both the scientific literature and popular press feature stories of success – and also of failure – with growing regularity.
Having acted as a study pathologist on several preclinical programs designed to evaluate the safety of cell-derived therapeutic agents, and having witnessed their potential efficacy, I can certainly share some of the excitement. However, my experience has also made me keenly aware of the massive cost (both financial and in terms of time) that can be incurred in the absence of a carefully crafted pathology protocol.
The regulatory pathway for conventional drugs and small molecules is clearly defined, with specified species and time requirements. In contrast, the requirements for preclinical safety and efficacy studies for cellular therapeutic agents tend to be much more fluid, with each study being considered on a case-by-case basis by the US Food and Drug Administration’s (FDA) Center for Biologics Evaluation and Research (CBER). Rather than having access to a predefined list of species choice and study type, companies can, and should, not only take advantage of pre-Investigational New Drug (IND) meetings, but also pre-pre-IND discussions with the agency to develop a customized protocol that provides scientifically sound data without breaking the bank.
A unique challenge facing this type of study is the fact that we are administering one living system (the cell line) into another (the animal model). The viability of the administered cells may be threatened by immune responses in the host, or by the dosing apparatus. The cells themselves are very sensitive to their microenvironment, and may assume a very different morphology from that in culture when they are placed in their intended location, or transported to other parts of the body. It’s therefore vital that pathologists demonstrate the presence of the cells in the tissues of the host animal during the study, show the continued viability of those cells, and confirm that the cells are differentiating into the intended cell type.
Know your targets
For each of these tasks, it is critical that we develop reliable biomarkers to confidently identify the administered cells, even if they take on a different morphology in differing microenvironments. Biomarkers may take the form of immunohistochemical (IHC) stains, antigenic determinants for use in quantitative polymerase chain reaction (qPCR) or in situ hybridization (ISH), or targeted growth factors produced as a result of endogenous stem and progenitor cell reprogramming.
The use of immunocompromised animals increases the range of available reagents for IHC and results in less off-target, non-specific, or background staining. While naturally immunocompromised strains of mice are readily available, their small size may render them unsuitable depending on the site of administration, size of dosing apparatus, or nature of the therapeutic agent. Large animal species may be better suited to your study and can be immunosuppressed. Immunocompromise was previously thought essential in ensuring the continued viability of the cells, but experience suggests that this is less critical than previously believed.
IHC markers – to confirm the cell of origin – may target the nucleus or nuclear matrix, the mitochondrial proteins, or cell-surface markers. There is no “one size fits all” answer here; a carefully developed method is an essential component of the early development program. The viability of administered cells can be proven by demonstrating continued (but controlled) mitotic activity among the cell population; Ki67 or PCNA may be successfully used in this scenario. Markers used to assess cell differentiation will depend on the target cell type; it can be challenging to develop a staining method that is species-specific for the administered cells with antibodies compatible with the research animal species.
I would recommend considering the use of the same antigenic determinants to target cell detection by qPCR. This can be invaluable as a highly sensitive screen for biodistribution of the cells. Relying on 5 µm sections and conventional IHC to scan a liver for a few migrating cells, for example, is rather like searching for a needle in a haystack. qPCR allows for a much larger volume of tissue to be examined. If qPCR is negative on the non-target tissues 28 days after cell administration, it is not unreasonable to store the tissue samples but drop the assay from the intermediate time points – a repeat assay can be performed at the final time point. Should any wandering cells be found at this time, the stored tissues are still available.
Pigment problems
Many of the more successful recent cell therapy programs have centered on ocular conditions. But the retinal pigment epithelium (RPE) can be a trying anatomical feature for the pathologist! The species-specific size and character of melanin granules should allow distinction between RPE cells and therapeutic cells on H&E-stained sections even if the cell line is pigmented, but such close scrutiny will prolong interpretation. Even with a non-pigmented cell line, confusion is likely when interpreting IHC sections; DAB precipitate is a similar hue to melanin, and bleaching the sections is likely to impact the sensitivity of the subsequent IHC stain. Immunofluorescence (IF) might be the answer (were it not for the fact that melanin shows autofluorescence!). Have you read a large GLP-study with IF? The only way to keep a permanent record of the staining is to photograph every section. An albino strain may just save your sanity.
Of course, IF can play a very important role during method development. The ability to demonstrate co-localization of staining can be a great advantage when presenting your proposed markers to the FDA. Having proved the robust and specific nature of your various markers in small-scale pilot studies using IF, you can justify using the same markers as conventional IHC stains on adjacent serial sections. This will give stable stained slides for archiving and negate the need to record each section photographically. Experience in our lab suggests that evaluating a study by IF takes three times as long as conventional IHC.
Model selection
When studies include an efficacy component, an animal model of the disease condition is required. Consider the suitability of your animal model carefully. For example, the commonly used mouse model for retinal degeneration is the rd1 mouse.
Homozygous mice have lost all photoreceptors by weaning – how do you ensure that the presence of administered cells is unlikely to be detrimental to adjacent surviving photoreceptors in a clinic situation? Be sure that you can predict the course of the condition in all animals: if the condition presents only in homozygous individuals, those animals must be identified prior to group allocation to avoid the awkward situation of having all the diseased animals in control (or treated) groups. In the case of retinal degeneration, the Royal College of Surgeons (RCS) rat may be a better model than the rd1 mouse, having a very predictable course of retinal degeneration.
Tissue triage
Because many of the therapies work on the premise that the cell line will continue to be viable in the patient for many years – or even a lifetime – a core tenet of preclinical study design for cell-based therapies is that all tissue should be preserved to allow for further scrutiny if problems arise further down the line. Tissues can be stored as wet tissues, in block, or on slides. To allow reconstruction of tissues, all sections cut should be appropriately labeled and retained. Unfortunately, this can create a logistical nightmare; serial 5 µm sections cut through a 1 mm block of tissue produce 200 sections. Although we may only stain 10 percent of the slides, the unstained slides must be stored for possible later evaluation; being uncovered, these sections must be stored in slotted slide boxes to protect the tissue. A 1 mm sample now occupies the space of two slide boxes.
So how can we control the number of slides? Either we need to reduce the number of tissues examined, the number of blocks processed, or the number of slides that we cut.
Firstly let’s consider the tissue list. These studies do not require examination of a full tissue list. Obviously you need to examine the site of implantation, the drainage lymph node, and any directly connected tissues (e.g. the brain has a direct connection to the eye via the optic nerve). You should also examine a variety of well-perfused organs (liver, kidney, spleen, lung, gonads). At a minimum you need to examine a single level of these off-target tissues to look for any evidence of toxicity, and to screen them for the presence of cells. If the cells remain at their site of implantation, or have only a transient lifespan in the host (operating through endogenous stem cells or progenitor cells), they are less likely to cause lesions at distant sites. Abnormal masses must also be examined to check for tumorigenicity. These could be screened using qPCR, but it may be more efficient to add them to the administration site IHC staining run for their time point. IHC is preferred for the site of administration, demonstrating the exact pattern of cell integration. Serial sections should be sequentially numbered. A predetermined pattern of slide selection identifies sections for H&E staining. The “best” level for the demonstration of the cells can then be selected by the pathologist (with a default level used if no cells are seen). Sections to either side of that level are then identified for IHC staining. Larger volume sites of administration could be trimmed into several portions and embedded in a single block, allowing a greater area to be examined on one slide, and the bulk of the tissue to be archived in the block.
Not all animals are equal
Consider treating control groups differently to cell-dosed animals. If no cells have been injected into a control group, there is no point doing an exhaustive tissue search to look for the presence of cells. You just need sufficient tissue to show both the background staining pattern – H&E and markers – and the background lesions if using a disease model. The remaining tissue from these animals can be stored wet, or taken to block without sectioning.
Does your cell line need a scaffold?
Several therapies are administered in the form of a sheet of cells on a matrix, adding another dimension to method development. The scaffold is essentially a medical device, and must be shown to be made of a biocompatible material. Ideally a scaffold may biodegrade after the cells have implanted but fragments may remain in situ, and it is unlikely that all traces of your scaffold will have disappeared from the tissues prior to the first time point; sections will include scaffold material. How does the material react with fixatives or histology processing reagents? Is the embedding medium sufficiently dense to avoid tearing of tissue sections by the scaffold fragments? These considerations should be thoroughly investigated prior to embarking on a large-scale preclinical study.
To summarize, I would say that examining the appropriate tissues at the conclusion of each time point is necessary to reap the full benefit of this “triaged” system. And this, together with DNA technologies, carefully selecting biomarkers and animal models, while creating more work in the lab and for the pathologist, could provide significant cost savings over the course of a study.
Julia is a senior veterinary pathologist at Charles River Frederick, Maryland site in the US, and has been working in the fields of toxicologic and diagnostic pathology for over 25 years. Julia is a member of the Executive Board of the International Society of Ocular Toxicology, and also serves on the Global Executive Steering Committee of the INHAND project and chairs the INHAND Special Senses organ working group. Julia also contributes to Charles River’s science blog, Eureka. Away from the microscope Julia works as a convergent media artist, using digital brushes to blend her own photography with layers of pure light, texture, and paint effects.




















