Infectious Disease Detective
A blood test to quickly decide if a viral or bacterial infection is the culprit causing disease could aid the quest to cut down on antibiotic misuse.
At a Glance
- Antibiotic resistance is a growing problem which has many experts worried, with a variety of possible solutions being put forward
- Identifying which patients have a bacterial infection and which have a virus using a blood test could help physicians make informed decisions on treatment
- An ELISA-based test that computationally integrates the measurements of several circulating host-proteins showed high accuracy in clinical studies and is being piloted n several hospitals
- A point-of-care platform and further clinical studies are planned to expand application to make it more accessible
The worrying problem of antibiotic resistance is frequently in the news, with global health forecasts over the last few years looking decidedly gloomy. Today, such predictions are becoming reality, and in some cases the situation is even worse than what was foreseen – the World Health Organization has named antimicrobial resistance a major threat to public health. A key factor in the rising resistance rates is antibiotic misuse. However, it must be acknowledged that misuse is not simply due to irresponsible prescribing, and is often driven by the difficulty in ascertaining the cause of the disease – bacteria or virus – especially in the early stages. The symptoms of many illnesses are similar, and lab tests such as C-reactive protein (CRP) or white blood cell count just aren’t accurate enough to tell apart bacterial and viral infections.
A lesser known issue is that this diagnostic challenge not only results in overuse of antibiotics, but in underuse as well. It is estimated that roughly one in five cases of bacterial infection are misdiagnosed, with serious consequences for some patients, especially the elderly and those in the developing world. Taking into consideration the limitations of current diagnostic approaches, our team decided to attack this problem from a different angle. We reasoned that over thousands of years, the human immune system has evolved distinctive responses to different pathogens. Pioneering studies have shown the potential of the immune system to effectively tell the difference between different infection types (1). This inspired us to develop a test which harnesses the sensitivity of the immune system to quickly distinguish between viral and bacterial infections, to aid in the diagnosis and treatment of disease, and to tackle the issue of microbial resistance.
Making theory reality
Now we had a theoretical starting point for developing our diagnostic test, we had to work out how to make it a reality, which took over four years. Firstly, we knew we wanted to identify immune response markers that are accessible and measurable even at the point of care. So we focused our search on proteins and other blood biomarkers, as these are easier and faster to measure than nucleic acids, especially in limited resource settings such as small hospitals and outpatient clinics. Secondly, we noted that most biomarker panels in use at that time contained bacterially-induced proteins, so we reasoned that including virally-induced proteins would create a more robust and accurate test.
With our demanding checklist of requirements in hand, we screened 600 human protein candidates. After multiple rounds of biomarker identification and validation, using both experimental and algorithmic approaches and a clinical study with over 1,000 participants, we identified several host-proteins that were differentially expressed. We then selected the most informative subset that included three proteins: TNF-related apoptosis-inducing ligand (TRAIL), interferon gamma-induced protein-10 (IP-10) and CRP. In line with our reasoning, the best subset included virally- and bacterially-induced proteins that display distinctive and complimentary dynamics during acute infections (Figure 1). We created an algorithm that integrates the levels of the three biomarkers to deliver a probabilistic score, which accurately predicts the cause of infection.
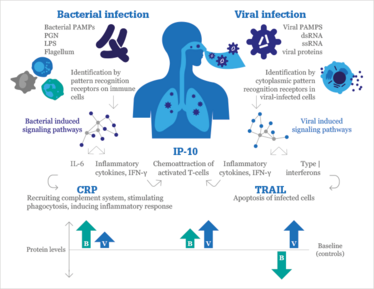
Figure 1. TRAIL, IP-10 and CRP participate in different signaling pathways and exhibit complementary dynamics in response to bacterial (B) and viral (V) infectious. PAMPS, pathogen-associated molecular patterns; PGN, peptidoglycan; LPS, lipopolysaccharide. Used under CC BY license, redrawn from original (2).
Putting it to the test
Our diagnostic test is fairly simple. Levels of the three proteins are measured in the hospital lab using ELISA, and our algorithm computes the likelihood of bacterial infection. We have shown the test to be robust across various pathogens, and our algorithm differentiates bacterial and viral infections with a sensitivity and specificity of over 90 percent (2). Today, the test is being piloted in several sites in Israel and Europe.
Now that the test is employed in working hospital labs, we’re seeing that it impacts patient management in several ways. The obvious clinical decision it can influence is antibiotic prescription – we believe our test is improving the ability to accurately identify the cause of infection, empowering physicians to make better informed treatment decisions. But that’s not all. Additional clinical decisions, such as requests for imaging data (e.g., chest radiographs, ultrasound and computed tomography) and work-ups, (e.g., multiplex PCR and lumbar punctures) are also influenced by the knowledge of the infection source. These procedures can be uncomfortable, and even pose risks to the patient, so the actionable information provided by our test has the potential to improve patient management and reduce healthcare costs beyond the “go/no go” decision about antibiotics.
Test results are currently available within a few hours. However, since we designed the test to require information on three proteins that can be readily quantified in the blood, we have the ability, and indeed are in the process of transforming it into a point-of-care test, which could return results in a matter of minutes. For pathologists and clinicians, we think our test will be regarded as a useful addition to the toolkit when piecing together the puzzle of infectious disease etiology.
Towards a superbugs solution
As our test is now CE marked and approved for clinical use in the EU, Switzerland and Israel, we intend to expand its availability in an early access program later this year. Further clinical studies are now underway across Europe and we are aiming to start clinical studies in North America. We believe our test has the potential to significantly impact antibiotic misuse, both by targeting those who need the drugs, and by preventing improper prescription. To quote the mission statement of the 2014 Longitude Prize; “We cannot outpace microbial evolution. A new broad-spectrum antibiotic, if applied with current methods, would eventually meet new forms of resistance. The overall solution involves a long-term path towards a more intelligent use of antibiotics enabling a future of more effective prevention, targeted treatments and smart clinical decision support systems.”
We hope that our diagnostic test, especially the point-of-care version, will play an important role in the solution to the problem of antimicrobial resistance.
- O Remilo et al., “Gene expression patterns in blood leukocytes discriminate patients with acute infections”, Blood, 109, 2066–2077 (2007). 2. K Oved et al., “A novel host-proteome signature for distinguishing between acute bacterial and viral infections”, PLoS One, eCollection, e0120012 (2015). PMID: 25785720.
Kfir Oved is a co-founder and CTO of MeMed, a biotechnology company based in Israel.
Eran Eden is co-founder and CEO of MeMed, a biotechnology company based in Israel.




















