Priming the Clinical Laboratory for Population Health
How a grassroots movement is positioning the laboratory at the forefront of healthcare
Khosrow Shotorbani, Jeremy Orr, Keren Landsman | | Longer Read
With an increasingly global society – not to mention a growing pandemic – the idea of population health is at the forefront of many medical minds. But who is responsible for population health? Is it the epidemiologists, the sociologists, or the politicians? A new movement, termed “Clinical Lab 2.0,” suggests that the laboratory is an integral part of population heath – and that laboratory medicine professionals can be leaders in the move from volume- to value-based healthcare. But what is Clinical Lab 2.0, and how does it position the laboratory at the apex of population health?
The meaning of Clinical Lab 2.0
An initiative of the Project Santa Fe Foundation, the Clinical Lab 2.0 movement is a grassroots effort to transform the role of the diagnostic laboratory to better support the objectives of population health and value-based healthcare. The effort, launched in 2016, is designed to promote more effective utilization of laboratory data in pursuit of the lab’s enormous potential for improving patient and population outcomes, reducing the total cost of care, and strengthening the patient and clinician experience.
The movement was born from a realization among a select group of laboratory leaders that our industry had reached a major inflection point. In other words, the past was no longer reflective of the future. We understood that the diagnostic lab’s value proposition needed to evolve dramatically to align with, and support, healthcare’s transition from volume to value. At the same time, it was clear that longstanding business models and conventional industry wisdom had not provided much room for innovation. Finally, as the commoditization of clinical testing has accelerated, it has become evident that hospital-based laboratories are at increasing risk of being sold or replaced by outsourced laboratory providers. And that’s why developing ways to add value to the lab have become critical.
In the simplest terms, Clinical Lab 2.0’s mission is to position the lab as the center of value-based care by promoting new strategies, models, and ideas to empower laboratory leaders – pathologists and management alike – to harness the data we collect in pursuit of population-level initiatives. These efforts can lead to substantial improvements in both outcomes and the cost of care. Underpinning this mission is a recognition that, although in vitro diagnostics account for just two cents of every dollar spent on US healthcare, lab results serve as the basis for over two-thirds of all medical decisions. Given the ubiquity of clinical testing, we believe the laboratory can positively impact virtually all aspects of healthcare and 100 percent of spending.
It has been four years since those laboratory leaders first met in Santa Fe (hence the name of the organization), and our message continues to gain traction both in the US and globally. We’ve created a nonprofit organization, launched four multi-institutional demonstration projects, hosted three additional closed-door colloquia, and produced three public workshops (all of which have been sold-out events) – and there is more to come. Our meetings continue to be critical to our movement by providing forums for a range of stakeholders to discuss the opportunities presented by the Clinical Lab 2.0 concept.
Extending the laboratory
Clinical Lab 2.0 represents an extension of the laboratory’s existing transactional model (Clinical Lab 1.0) to incorporate and reflect quantitative value around the total cost of delivery and cost avoidance. Whereas 1.0 is reactive and focused on “sick care” and de-escalation, 2.0 concentrates on early detection, early escalation, intervention, and prevention (see Tables 1 and 2).
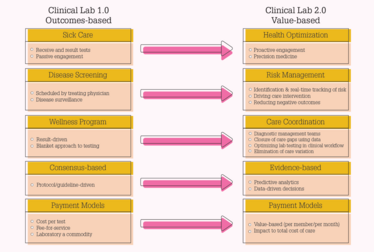
Table 1. Contrasting Clinical Lab 1.0 with Clinical Lab 2.0.
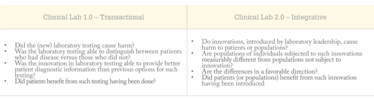
Table 2. Testing the utility of lab services and the value of Project Santa Fe recommendations.
In 2017, we authored an article that we hoped would change the conversation about the potential of the clinical lab (1). We asserted that, in traditional business and care models, the clinical lab has been viewed primarily as an ancillary and increasingly commoditized departmental function. In the 2.0 model, the lab’s aggregated data provides vital longitudinal touchpoints to support the full spectrum of integrated health care. Because the lab generates data regardless of where, when, or how the patient receives care, we can serve as a repository of actionable information across the entire care continuum.
Clinical Lab 2.0 can support pre-diagnostic identification and closure of care gaps, as well as deliver post-diagnostic computations of aggregated longitudinal data to enable a range of insights and actions. These include clinical prevention, programmatic clinical interventions, and optimization of diagnostic and therapeutic management. Our goals? Improved patient and population outcomes and management of population risk.
In effect, Clinical Lab 2.0 views lab personnel as “first responders.” They’re the first to see these critical important data and the best-equipped to understand the implications. As such, they’re optimally positioned to manage population health in value-based care.
My Clinical Lab 2.0 story
Clinical Lab 2.0 has no borders – it’s truly a global movement. I’ve been excited to see the level of interest and engagement our efforts have elicited in diverse healthcare settings around the world. I’ve heard about the concerns and challenges faced by healthcare systems globally – and what I’ve learned is that, regardless of the setting, the fundamental principles of Lab 2.0 are universal in their application. Labs can play a critical role by providing population risk stratification relative to the known prevalence of chronic conditions, identifying care gaps and predicting clinical risk, identifying high-risk patients before they are admitted into emergency room or hospital, and facilitating early intervention between care providers and patients. These capabilities and their implications resonate globally.
The Lab 2.0 integrative model cannot exist without a solid Lab 1.0 foundation. The models are iterative and interconnected. In envisioning the lab as the first responder, we’re saying that the lab is the first to become aware of a clinical need and therefore in the best position to provide leadership in addressing that need. Reducing the time to diagnosis can help with diagnostic optimization and appropriate laboratory test utilization, which, in turn, leads to care optimization, therapeutic optimization, and appropriate screening and surveillance.
If we don’t get the first step – identifying actionable clinical information at the point at which it is generated – right, the entire continuum of care becomes suboptimal, and that can cause significant patient harm. The lab can be the catalyst for improving population health outcomes, reducing the overall cost of care and, importantly, empowering health systems to successfully manage the financial risk of providing value-based care. The central advantage we possess is the ability to produce scientifically measured, structured data at each touchpoint on the care continuum. That means the information we generate is clinically actionable with zero latency.
From obstacles to opportunities
We’ve identified a number of barriers or obstacles that can impact the transition to Lab 2.0. These include:
- Lack of a common language among providers, data analysts, health systems, and payers with respect to certain clinical conditions and lab results
- Lack of models for comparison and benchmarking
- The inability of existing laboratory information systems to integrate data or provide information for clinical decision support; current systems tend to support only revenue cycle and contract pricing data
- Lack of outcomes-based evidence for laboratory-led innovation
- Difficulty integrating laboratory insights into the existing clinician workflow
- Lack of aligned incentives
- Inadequate leveraging of laboratory data into actionable information, including the absence of detailed data-sharing agreements
- Lack of access to capital for in-system laboratories versus the for-profit sector of laboratory industry
- Lack of access to new and necessary skill sets
- Limited understanding of the laboratory’s potential among health system leaders and inadequate engagement of same
- No playbook for providing Lab 2.0 leadership
The Lab 2.0 initiative helps the industry overcome these barriers by emphasizing three fundamental pillars of transformation:
- Leadership: Helping clinical lab leaders embrace a new leadership mindset that extends beyond the four walls of the laboratory.
- Standards: Measuring what matters – that is, the development of new measurements and benchmarks that support a new clinical value proposition.
- Evidence: Developing multi-institutional demonstrations to show how laboratory medicine and pathology affect population health and align with the drivers of value-based care. Our projects focus on providing outcomes-based evidence and producing roadmaps that all labs can follow.
Our Project Santa Fe colleagues and participants have encountered many of the opportunities generated by a more engaged and integrated lab. Here are just a few that have been presented in the recent literature:
Diabetic patients (with comorbidity): In most countries, attempts to de-escalate the impact of diabetes don’t occur until morbidity is severely advanced, typically when the patient’s A1C level is over 9 and the kidney function (EGFR) is below 60. Generally, this means irreversible stage 3 kidney failure. However, if at-risk patients are identified early – when their A1C is 5–7 and EGFR is between 90 and 60 – we can manage their care to improve outcomes and reduce downstream cost. The ability to identify at-risk patients in the pre-diabetic stage can help avoid the progression of the disease which, if uncontrolled, can cost an average of $10,970 per case (2).
Urinary tract infections: Laboratory-provided insights into urinary tract infections managed in the emergency room (ER) not only diagnose the acute condition, but also offer clues to improving treatment and identifying patients with recurrent infections. These insights “could result in more appropriate drug treatment, improved resource allocation, and decreased ER costs for integrated health systems (3).”
Cost-effective drug therapy regimens for chronic disease: Laboratories are beginning to understand the value of having pharmacists on their staff. These experts can help with antibiotic stewardship and identify appropriate treatments for chronic diseases – especially those that, like rheumatoid arthritis and chronic reoccurring infections, require long-term, high-cost therapy. “To manage these diseases, the cost of drug treatment, monitoring of drug therapy regimens, and treatment adjustments for empiric therapy require post-analytic interpretation of laboratory results, along with drug therapeutics knowledge (3).”
Pregnancy: For women who don’t receive routine care – for instance, those on low incomes or without insurance – laboratories can identify pregnancies early, avoid treatment options that could present a pregnancy risk, and monitor prenatal testing patterns and results to identify high-risk pregnancies and women in need of more intensive prenatal care (3).
Opioids and benzodiazepines: We need innovative approaches to tackle the ongoing opioid crisis. “As stewards of health analytic data, laboratories are uniquely poised to approach the opioid crisis differently,” says one study (4). The pilot study aimed to “bridge laboratory data with social determinants of health data, which are known to influence morbidity and mortality of patients with substance use disorders.” The study found that co-use is largely determined by the patient’s providers, with increasing age and geographic area also predicting co-use. “The prominent geographic distribution of co-use suggests that targeted educational initiatives may benefit the communities in which co-use is prevalent. This study exemplifies the Clinical Lab 2.0 approach by leveraging laboratory data to gain insights into the overall health of the patient.”
The future of Clinical Lab 2.0 is somewhat academic, but with a sense of agility and urgency. Our vision is to share knowledge through publications and key partnerships, to continue to build the evidence base with expanded multi-institutional demonstration projects, and to continue to host annual scientific colloquia and produce educational workshops. Project Santa Fe Foundation is a member-driven organization. Obviously, our movement cannot achieve its objectives alone – so key partnerships are a critical component of our future activities. These relationships will help us broaden our reach, engage industry partners in the in vitro diagnostics and informatics space, and potentially help influence policies that determine the direction of healthcare. Ultimately, our goal is to create a tipping point that elevates the value of the clinical lab, domestically and globally, as healthcare transitions from volume to value and from sick-care to well-care.
How to implement Clinical Lab 2.0
Become stewards of data. Create patient-centric longitudinal data sets that make clinical sense. This will support population risk stratification, identification of care gaps, and early identification of high-risk patients. Laboratories enable actionable signals to manage the risks of unfavorable outcomes and inordinate financial resource use. This fundamental step, combined with domain knowledge of pathology, will begin the conversation with key stakeholders outside of the lab.
Get outside the four walls of the lab. Lab leaders must be able to engage the C-suite in discussions about how the lab can impact enterprise-level initiatives and play a pivotal role in population health, value-based care, and mitigating financial risk. We must be able to use C-suite language and address organizational imperatives.
Take a seat at the table. Actively engage in helping design future healthcare delivery models that use the predictive value of the clinical lab data for clinical intervention, prevention, and cost avoidance. The lab must be at the table – perhaps even at the head of the table – to achieve better, more cost-effective care.
Demonstrate value. We need to prove to the C-suite that the lab’s value extends beyond simply costs per unit. Look for short-term wins. We must align ourselves with key enterprise objectives by demonstrating the value we can deliver in areas that hospital leaders care about: outcomes, total cost, clinical risk, financial risk, affordability, and increased access. If we fail, we become a target of outsourcing.
We need to think big but act small. We don’t have to boil the ocean to add new value – just getting out of the lab and telling a different story is mission-critical. To start, you can mobilize clinical data in a way that makes sense for your local healthcare needs. For example, you could add basic delta checks on some critical assays, start reporting that change to your clinical colleagues, and seek their input.
But we can’t do this in a vacuum. Lab 2.0 requires strategic and operational planning that can demonstrate the tangible value of the clinical lab for customers we may never have served before. Don’t encumber the Lab 2.0 way of valuation with old ways of doing business. Enterprise health organizations must find ways to improve clinical outcomes, reduce financial risks, and improve patient satisfaction. Otherwise, we’ll be at the mercy of inadequate reimbursement models.
A quote from James Crawford, our Project Santa Fe Foundation Chairman of the Board, sums it up best: “There has never been a better time to demonstrate the value of laboratory medicine and pathology in the delivery of healthcare – but it must be quantitatively proven and attributable to the lab’s contribution.”
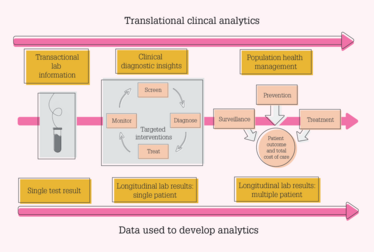
Remodeling of laboratory information to provide clinical diagnostic insights using longitudinal data (3).
We would also like to acknowledge the Project Santa Fe Foundation Board of Directors’ institutions: Geisinger Health System, Henry Ford Health System, Intermountain Healthcare Central Laboratory, Kaiser Permanente Northern California, Mayo Clinic Laboratories, Northshore University HealthSystem, Northwell Health, TriCore Reference Laboratories, and The Robert Larner, M.D. College of Medicine, University of Vermont.
Labs, Population Health, and COVID-19
By Khosrow Shotorbani
The question you may be asking is: as guardians of public health, what is the lab’s role in the COVID-19 pandemic? Obviously, our ability to serve as leaders goes beyond our duty to provide timely, accurate testing.
The four points we need to highlight – and illustrate by our actions – are:
- The laboratory is the first to know with real-time results.
- Laboratories are the first responders providing recommendations and developing new strategies.
- Laboratories are the “epicenter of informatics.” with insights around disease patterns and predicting outbreaks.
- Laboratories should serve as the “command center” managing this pandemic by developing guidance as to who should be tested and when.
In the COVID-19 pandemic response, the lab takes center stage. I have been humbled as I’ve witnessed my colleagues across the country rise to the challenge. In my opinion, it’s impossible to overstate the impact of the laboratory at this time.
I’ve been asked, “What is the role of Clinical Lab 2.0 in managing this pandemic?”
The Clinical Lab 2.0 model is based on three key actionable pillars:
- Leadership outside the clinical laboratory
- Clinical Lab 2.0 new standards: measuring what matters to provide actionable data that can lead to objective key results
- The science of laboratory medicine: focusing on not just the analytical components of lab medicine, but also the pre- and post-analytical stages
The Clinical Lab 2.0 model argues that laboratory medicine professionals must assume a leadership role outside the lab and engage their health system’s stakeholders and public health agencies. Obviously, we have to set up testing to keep up with demand – a key task that, at this point, remains challenging. Clinical Lab 2.0 can then potentially mine longitudinal data (laboratory results, patient demographics, and any pre-existing or past conditions) to proactively determine which patients are potentially at risk of comorbidities. Labs can help their health systems risk-stratify their populations based on historical conditions, such as respiratory syndromes or infections, chronic diseases like diabetes mellitus, or cancer leading to immunosuppression.
It’s important to remember that a negative COVID-19 test result doesn’t entirely eliminate a patient’s risk. Not only are false-negative results possible, but any patient who has not yet been infected remains vulnerable. Labs can identify a high-risk patient pool, then partner with providers and state agencies to develop targeted isolation strategies for prevention and intervention focused on outcome.
COVID-19 has undoubtedly raised the critical, urgent, and quantitatively relevant value of the clinical lab and its clinical assets globally. The lab is the centerpiece of healthcare delivery and provides a method to triage care, as opposed to being an ancillary cost center. The clinical lab is the catalyst managing population health, helping to flatten the curve of not only COVID-19, but also chronic conditions.
We also cannot forget the role of the lab in returning infected patients – and, indeed, the population as a whole – to normal life. Who is infectious? Who is immune? Who can go back to work and who must remain in lockdown? This is an especially vital function as it relates to healthcare workers and first responders on the front lines. Furthermore, the data we gather – and the tests we conduct – are critical to further evaluating the effectiveness of treatments and vaccines, and to detecting (and ideally preventing) future waves if COVID-19 becomes a seasonal affliction. It’s our job to provide global surveillance so that not just individual patients, but the entire population, can be protected.
In this pandemic, global healthcare faces the ultimate challenge. Now, more than ever, the tangible value of the clinical laboratory – and the unsung heroes who keep it running every day – is self-evident. The lab’s potential impact doesn’t end when we release a result; rather, that’s where it begins!
A Clinician’s Perspective: COVID-19 and the Lab’s Evolving Role
By Jeremy Orr
During the early part of the pandemic, laboratorians mobilized to provide timely, accurate testing for individual patients. In places where testing was limited, lab personnel sometimes enforced prioritization criteria. Fortunately, in many (though not all) parts of the world, tests are now available in greater quantities and rationing is no longer an issue. So it’s natural to ask: what lies ahead for the lab as the next stages of the pandemic unfold?
First, let’s acknowledge that none of us know for certain how the next few months will go. Different regions are at different points on their case growth curves – and the shapes of those curves are dependent on the circumstances. Will there be a rebound in places where an apparent peak has been reached? Will we see COVID-19 take on seasonal characteristics like influenza? Will containment efforts evolve or corrode? What role will herd immunity play? When will there be a viable vaccine? We just don’t know the answer to these questions.
Despite the uncertainty, the laboratory will continue to play a central role – but the nature of that role will evolve. Here are some of the potential future use cases – and how the lab may fit in:
- Patient triage and population health efforts. For patients who have already tested positive, laboratorians are in a strong position to provide risk stratification to guide disposition and follow-up protocols.
- Contact tracing – a best practice in epidemiology, but also a resource-intensive one. Not every COVID-19 positive patient will have complete contact tracing. Because clinicians operate 1:1, they often can’t see the connections between events. Labs can see all the data and map the temporal and geospatial relationships between events. There is a long history of labs reporting this data to public health agencies for surveillance purposes, but they can do more. Even tracing within a health system or locality can help prioritize contact tracing and mitigate disease spread.
- Antibody testing. It’s fraught with challenges, but has been used for other infectious diseases and will be used for COVID-19 to assay immunity at both the individual and population level. Given the interpretation pitfalls, lab expertise will be needed to guide policy and implementation.
- Vaccine prioritization. An effective COVID-19 vaccine will be critical to long-term containment. But, in the early days of any vaccine, access is often limited and we will have to decide who goes first. Essentially, it’s a risk/benefit ratio, and labs – the center of the care data flow – are in an excellent position to help.
- Return to routine. We all know that routine care, including cancer screening and chronic disease management, is being delayed and deprioritized for this phase of the pandemic. How do we get back to par? As routine care efforts rebound, the lab can again play a central role in helping providers understand who needs care most urgently. Who should be at the front of the cue for a colonoscopy or a diabetes check-up? Labs provide critical clues.
Central to all of these use cases is the careful and informed interpretation of data familiar to the lab. Of course, lab personnel cannot alone be responsible for surveying all data available to them for the purposes of powering these use cases – but they don’t need to. Newer technologies, including machine learning, are maturing just in time to help. Newer algorithms (full disclosure: including some developed by my company) can systematically analyze structured data and lab results to flag the patients at highest risk for COVID-19 complications, cancers, chronic disease complications, and more. The natural place for running these complications is in the lab – why? Because labs have both the data and the natural expertise to translate insights back to providers.
Jeremy Orr is a practicing, board-certified family physician and Chief Executive Officer and Chief Medical Officer of Medial EarlySign, Aurora, Colorado, USA.
Protecting the Population
How “behind the scenes” workers are safeguarding the world’s health during the COVID-19 pandemic
Michael Schubert interviews Keren Landsman
Can you tell us a little bit about your work?
I’m a doctor specializing in epidemiology and public health. Ordinarily, I work in two places – in the epidemiology department of the Israeli Ministry of Health and in the Levinsky Clinic, a free sexual health clinic where we test and treat people from all kinds of socioeconomic backgrounds. At the moment, the clinic is closed and I’m working full-time at the Ministry of Health to deal with the COVID-19 pandemic.
What is the current COVID-19 situation in Israel?
We’re doing pretty well on a global scale. The Ministry of Health moved very quickly to decide on a curfew, stop all flights abroad, and initiate social distancing protocols. But that’s not to say we aren’t facing issues here; we have over 9,000 confirmed cases and over 50 deaths to date – but we studied the curves and tried to learn from the events in other countries. We had China, South Korea, and Italy to learn from before COVID-19 hit Israel, so we worked around the clock to purchase and produce supplies, source ventilators, and prepare special sections in each hospital for COVID-19 care. New cases are still being diagnosed everywhere, but Israel’s upward trajectory is slow compared with other countries, so I am cautiously optimistic.
Globally, how well is the pandemic being handled?
That’s a very tricky question because each country has a different approach. We don’t have a global health department to coordinate efforts worldwide. The closest authority we have is the World Health Organization, but their function is to make recommendations, rather than to take action.
I think the biggest thing we need to learn from this pandemic is how to cooperate internationally on health. We need to understand that viruses do not recognize borders. If we want to stop the next outbreak before it becomes a pandemic, we all need to work together – regardless of a country’s size, population, politics…
How are “behind the scenes” healthcare professionals contributing?
There’s a lot of work being done that isn’t very visible. We all know about the doctors and nurses on the front lines. We see pictures of them in the media every day, wearing masks (if they’re lucky) and treating patients. But there are a lot of people you don’t see: pathologists, laboratory staff, radiologists, technicians, epidemiologists, cleaners, and more. All of us are working together to mitigate the impact of COVID-19.
In any battle, you see the soldiers on the front lines, but you don’t necessarily see the hard workers behind them – logistics, supplies, even the person sewing the buttons onto their uniforms. But, as in any battle, one of the most important things I’ve seen in this pandemic is how important it is to have someone or something to fight for. Every battle, even this one, will end, and we all need something to go home to – a family, a partner, a pet, or even just the comfort of your own bed, which I know many healthcare professionals are working too hard to enjoy right now.
How do you think the move from volume- to value-based care will affect COVID-19 testing and management?
In Israel, we are under massive public pressure to increase the volume of testing. The public want us to test as many people as we can, as often as we can, regardless of how sensitive or specific the tests are. As you can imagine, I have a little bit of a problem with that!
I think the general public views testing as very black-and-white. Many common medical tests are presented to patients as either positive or negative; you either have the condition or you don’t. Of course, expert diagnosticians know that isn’t the case – and COVID-19 is no exception. Someone who tests negative for SARS-CoV-2 today might test positive tomorrow. The result might be a false positive or negative; many currently available tests have low sensitivity or specificity. We don’t need more volume; we need more value. We need better tests.
That’s not to say we shouldn’t be testing more people – it’s just that I don’t think we should be taking that step right now. First, we need accurate tests – for both disease diagnosis and antibody screening – and then we should roll those tests out to the population. Only then can we begin lifting the precautionary restrictions and returning to our normal lives.
In your opinion, what does the near future look like?
This is my favorite kind of science fiction – near-future science fiction!
Why do I call it “science fiction?” Because the truth is, nobody knows what even the near future holds. We first heard about SARS-CoV-2 in December. The virus didn’t even have a name until February. We’ve only been acquainted with it for four months. There are a lot of theories and guesses at the moment, but there’s no such thing as an accurate projection right now. I would caution everyone to be wary of people who claim to know what’s going to happen, because no such thing is possible.
What I can tell you is that, at some point, the immediate threat of the pandemic will die out, the restrictions will be lifted (although, again, each country has a different approach to achieving that), and we will go back to living our lives. But SARS-CoV-2 won’t disappear. We will have to learn to live with the virus. There will be a “new normal,” although it’s impossible to say how that might look.
We will also need to truly grasp the fact that there will be another pandemic – we just don’t know when. It might be a century, a decade, or even just a year or two from now. Nobody knows. But, because future pandemics are an absolute certainty, I hope that we learn to work together as a global community. The only way to mitigate the impact of a future pandemic is to coordinate health efforts around the world as soon as a new disease emerges. If we take one positive from the COVID-19 pandemic, I hope it’s a truly global health system.
As an epidemiologist, what has your professional experience been?
Too many people have become experts in epidemiology in the last three months! I see graphs everywhere. I see people making all kinds of assumptions without sitting through a single epidemiology lecture. Everyone suddenly knows everything about pandemics – the Dunning-Krueger effect at its worst!
It has been interesting to see how many of my professional colleagues have developed a deep respect for epidemiologists. I’m sure the same is true for pathologists and laboratory medicine professionals, who have come to the forefront now that screening and diagnosis are of the essence. The laboratorians I know are treating this virus as cautiously as possible and striving to serve patients while avoiding infection.
If I could offer my colleagues throughout science and medicine one piece of advice, it would be to communicate very clearly about what is in their area of expertise – and to be equally clear about what is not. I think people tend to assume that if we are experts in one subject, we must be experts in related subjects – and that isn’t true at all. It’s okay to have opinions and to theorize – but, when you are a healthcare professional, your opinion counts more in the current crisis. So be clear, stay calm, and stay safe.
Keren Landsman is a public health specialist. She is a member of Mida’at, a public health non-governmental organization, and works as an epidemiologist in the Israeli Ministry of Health and as a physician in the Levinsky Clinic, Tel Aviv, Israel.
- JM Crawford et al., “Improving American healthcare through ‘Clinical Lab 2.0’: a Project Santa Fe report”, Acad Pathol, 4, 2374289517701067 (2017). PMID: 28725789.
- TM Dall et al., “The economic burden of elevated blood glucose levels in 2012: diagnosed and undiagnosed diabetes, gestational diabetes mellitus, and prediabetes”, Diabetes Care, 37, 3172 (2014). PMID: 25414388.
- K Swanson et al., “Improving the delivery of healthcare through clinical diagnostic insights: a valuation of laboratory medicine through ‘Clinical Lab 2.0’”, J Appl Lab Med, 3, 487 (2018).
- JS Warrington et al., “Integrating social determinants of health and laboratory data: a pilot study to evaluate co-use of opioids and benzodiazepines”, Acad Pathol, 6, 2374289519884877 (2019). PMID: 31700992.
President and Executive Director of Project Santa Fe Foundation, CEO and founder of Lab 2.0 Strategic Services, LLC, and a Clinical Laboratory 2.0 industry advocate.
Practicing, board-certified family physician and Chief Executive Officer and Chief Medical Officer of Medial EarlySign, Aurora, Colorado, USA.
Keren Landsman is a public health specialist. She is a member of Mida’at, a public health non-governmental organization, and works as an epidemiologist in the Israeli Ministry of Health and as a physician in the Levinsky Clinic, Tel Aviv, Israel.