Case of the Month
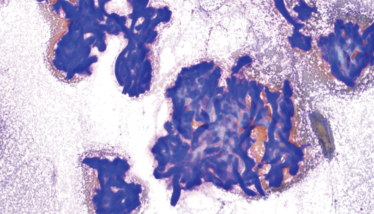
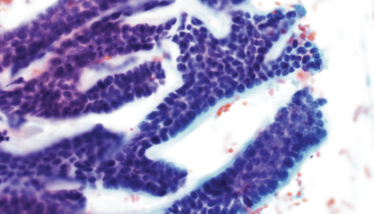
A 61-year-old woman presented with a 1 cm left postauricular mass that she had initially noticed three months earlier. On imaging, the lesion appeared to be well-circumscribed. A fine needle aspiration was performed and yielded cellular smear preparations, of which representative findings are displayed in the images below.
What is the most likely diagnosis?
a. Cellular pleomorphic adenoma
b. Basal cell adenoma
c. Adenoid cystic carcinoma
d. Polymorphous adenocarcinoma
e. Epithelial-myoepithelial carcinoma
Click here to register your guess.
We will reveal the answer next month.
Do you have an interesting case that you would like us to feature? Email it to [email protected].
The Case of the Month series is curated by Anamarija M. Perry, University of Michigan.
D. T-cell prolymphocytic leukemia
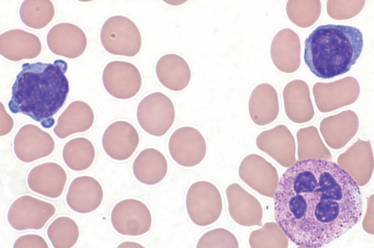
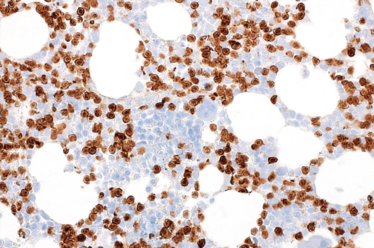
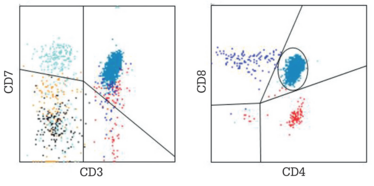
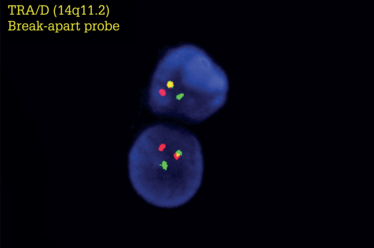
T-cell prolymphocytic leukemia (T-PLL) is an aggressive T-cell leukemia that involves peripheral blood, bone marrow, lymph nodes, spleen, liver, and occasionally skin. On peripheral blood smear, the prolymphocytes are small to medium-sized, with round to irregular (and occasionally cleaved) nuclei, visible nucleoli, and cytoplasmic blebs. Immunophenotypically, T-PLL cells are positive for CD3, CD2, CD5, CD7, TCL1, and CD52. Most cases are CD4-positive (rarely CD8-positive); double CD4/CD8 expression (as observed in this case) is seen in around 25 percent of cases. This “double-positive” phenotype is not usually observed in other peripheral/post-thymic T-cell lymphomas. The most common cytogenetic abnormality, seen in 80 percent of patients, is inv(14)(q11.2q32.1) or, rarely, variant t(14;14)(q11.2q32.1). These lead to juxtaposition of the T-cell receptor TRA at 14q11.2 with the TCL1A and TCL1B genes at 14q32.1, activating these genes. T-PLL is an aggressive disease with median survival of one to two years. The patients usually respond to treatment with anti-CD52 monoclonal antibody (alemtuzumab).
Differential diagnosis of T-PLL includes T-lymphoblastic leukemia/lymphoma (T-LBL). In contrast to T-PLL, T-LBL is an immature neoplasm, usually expressing TdT or CD1a. Differential diagnosis from other mature T-cell leukemias/lymphomas (such as T-cell large granular lymphocytic leukemia, adult T-cell leukemia/lymphoma, mycosis fungoides-Sezary syndrome, or hepatosplenic T-cell lymphoma) can be challenging due to overlapping morphologic and immunophenotypic features. Morphologic evaluation, in combination with different ancillary studies and clinical correlation, is usually needed to resolve differential diagnosis.
Contributed by Laura Baugh and Lina Shao, Department of Pathology University of Michigan, Ann Arbor, Michigan, USA.
- SH Swerdlow et al., WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th edition. IARC: 2017.