Plasma cell enrichment can increase FISH sensitivity for detecting high-risk cytogenetic abnormalities, which may help improve risk stratification and patient management when combined with clinical follow-up data (1)
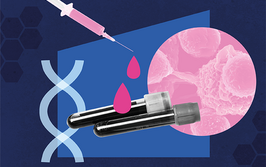
A Glimpse of Multiple Myeloma

A cancer of the plasma cells, multiple myeloma (MM), is a heterogeneous disease in which patients have one common characteristic – almost all exhibit karyotypic abnormalities, with some studies showing an average of 8–10 changes present at diagnosis (2,3). The most common of these are translocations and hyperdiploidy (4) – but they do not stand alone; secondary cytogenetic events in MM may warrant repeat cytogenetic testing (5).
Cytogenetic Testing

Cytogenetic testing is one component in the assessment of MM and related conditions. One reason is risk stratification; knowing a patient’s disease-specific mutations may help in understanding prognosis (5,8). Karyotypic abnormalities, such as t(6;14) or t(11;14) translocations or hyperdiploidy, are considered standard risk. t(4;14), t(14;16), t(14;20), and del(17p) place patients in the high-risk group according to Mayo Clinic mSMART 3.0 risk stratification guidelines (9,10,11,12). Standard risk is defined as having an indolent course of disease and lengthy survival, and high risk is defined as experiencing a more aggressive course and shorter survival (11,12). Both the National Comprehensive Cancer Network (NCCN) and the International Myeloma Working Group (IMWG) currently recommend cytogenetic analysis for all MM patients at the time of diagnosis (5,8).
IgH Translocations in MM

IgH translocations most likely occur in 50 to 70 percent of all MM cases (6). These translocations result in derivative chromosomes that may place enhancers next to oncogene promoters – thus increasing the activation of oncogenes (7).
Approaches to Cytogenetic Testing

1. Conventional karyotyping is widely available and commonly used, but requires cells to be in metaphase (13,14) – a unique challenge in myeloma due to the cells’ low proliferation rate – and has a success rate of only 30–40 percent in detecting cytogenetic abnormalities in MM (14,15,16).
2. Fluorescence in situ hybridization (FISH) can be used on plasma cells in interphase and has a high (>90 percent) detection rate when using enriched plasma (16). Additionally, FISH analysis can detect IgH translocations not visible using conventional karyotyping (10,17). However, its success depends heavily on probe selection (7,18); IgH break-apart probes can help clearly identify the presence of an IgH translocation, while dual-color, dual-fusion probes can be used to definitively identify the specific type of IgH translocation (19,20).
3. Next-generation sequencing (NGS) may perform as well as FISH and may provide a more comprehensive, cost-effective approach in the near future (21,22).
Enhancing Sensitivity

The College of American Pathologists recommends improving sensitivity with either plasma cell enrichment or cytoplasmic immunoglobulin-enhanced FISH (1,23). Plasma cell enrichment can improve detection of cytogenetic abnormalities threefold when used with FISH and may be achieved in one of three ways:
1. Flow cytometric analysis is useful for comparison and quality control of plasma cell enrichment to ensure adequate CD138 expression if performed before plasma cell separation (24).
2. Magnetic-activated cell sorting (MACS) enables positive CD138 selection (25) but with MACS, timing is important; cells may lose CD138 expression outside the bone marrow environment (26). One analysis found that MACS-enriched plasma cell concentration from a single specimen declined from about 58 percent on day two to about 13 percent on day eight (24).
3. Fluorescence-activated cell sorting (FACS) offers more pure plasma cell separation than MACS and permits the analysis of specimens with decreased CD138+ expression (24).
Because aspirates typically do not contain a large number of plasma cells, timing is sensitive and multiple tests may be needed; close communication among laboratories, pathologists, and oncologists is crucial (27).
- G Lu et al., Arch Pathol Lab Med, 137, 625 (2013). PMID: 23627452.
- T Nilsson et al., Br J Haematol, 120, 960 (20063). PMID: 12648065.
- WJ Chng et al., Genes Chromosomes Cancer, 45, 1111 (2006). PMID: 16955468.
- J-P Capp, R Bataille, Front Oncol, 8, 355 (2018). PMID: 30250824.
- R Fonseca et al., Leukemia, 23, 2210 (2009). PMID: 19798094.
- D Saxe et al., Int J Lab Hematol, 41, 5 (2019). PMID: 29971938.
- BA Walker et al., Blood, 121, 3413 (2013). PMID: 23435460.
- National Comprehensive Cancer Network, Available at: https://bit.ly/3jkMWnC.
- A Dispenzieri et al., Mayo Clin Proc, 82, 323 (2007). PMID: 17352369.
- P Kapoor et al., Mayo Clin Proc, 85, 532 (2010). PMID: 20511484.
- JR Mikhael et al., Mayo Clin Proc, 88, 360 (2013). PMID: 23541011.
- SK Kumar et al., Mayo Clin Proc, 84, 1095 (2009). PMID: 19955246.
- CY Soekojo et al., Clin Lymphoma Myeloma Leuk, 19, e470 (2019). PMID: 31171473.
- SV Rajkumar et al., Cancer Genet Cytogenet, 113, 73 (1999). PMID: 10459351.
- C Aydin et al., Indian J Hematol Blood Transfus, 36, 284 (2020). PMID: 32425379.
- O Pozdnyakova et al., Cancer Genet Cytogenet, 189, 112 (2009). PMID: 19215792.
- WJ Chng et al., Leukemia, 28, 269 (2014). PMID: 23974982.
- FM Ross et al., Haematologica, 97, 1272 (2012). PMID: 22371180.
- T Smol, A Daudignon, Cytogenet Genome Res, 153, 18 (2017). PMID: 29040969.
- JR Cook et al., J Mol Diagn, 8, 459 (2006). PMID: 16931586.
- I Cuenca et al., Blood, 136, 13 (2020).
- M Manzoni et al., Cancers, 12, 1332 (2020). PMID: 32456143.
- JD Khoury et al. (2015). Available at: https://capatholo.gy/37vlWw7.
- L Hartmann et al., Am J Clin Pathol, 136, 712 (2011). PMID: 22031309.
- N Put et al., Genes Chromosomes Cancer, 49, 991 (2010). PMID: 20662075.
- M Zlei et al., Exp Hematol, 35, 1550 (2007). PMID: 17889722.
- TJ Pugh et al., Cancer Genet, 228-2291, 184 (2018). PMID: 30393007.